Istanbul Retina Institute
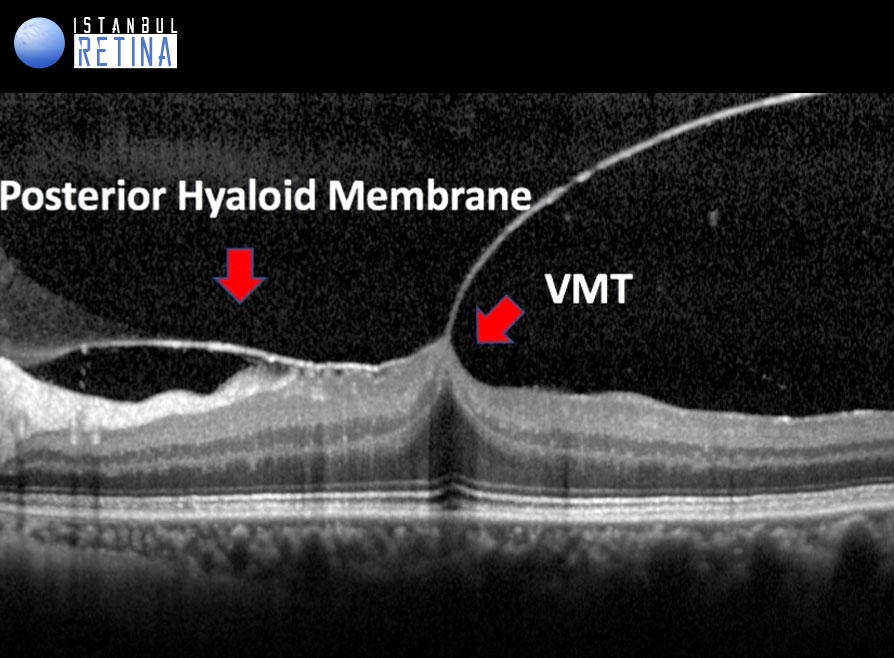
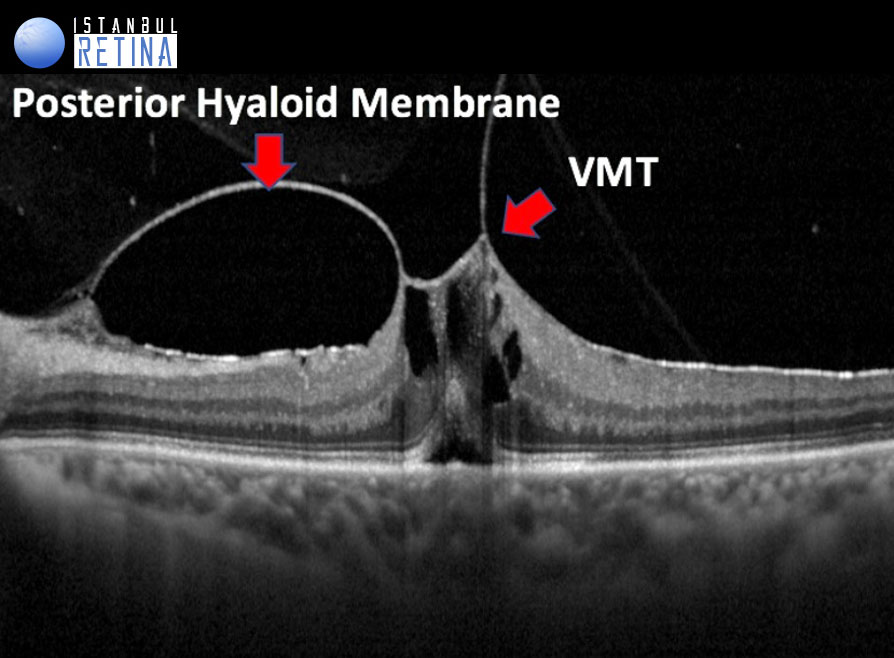
The progression of PVD can lead to periods of excessive traction on the macula. Such traction can result in anatomic changes in the contour of the foveal surface, intraretinal pseudocyst formation, elevation of the fovea from the RPE, or a combination that typically results in reduced or distorted vision.
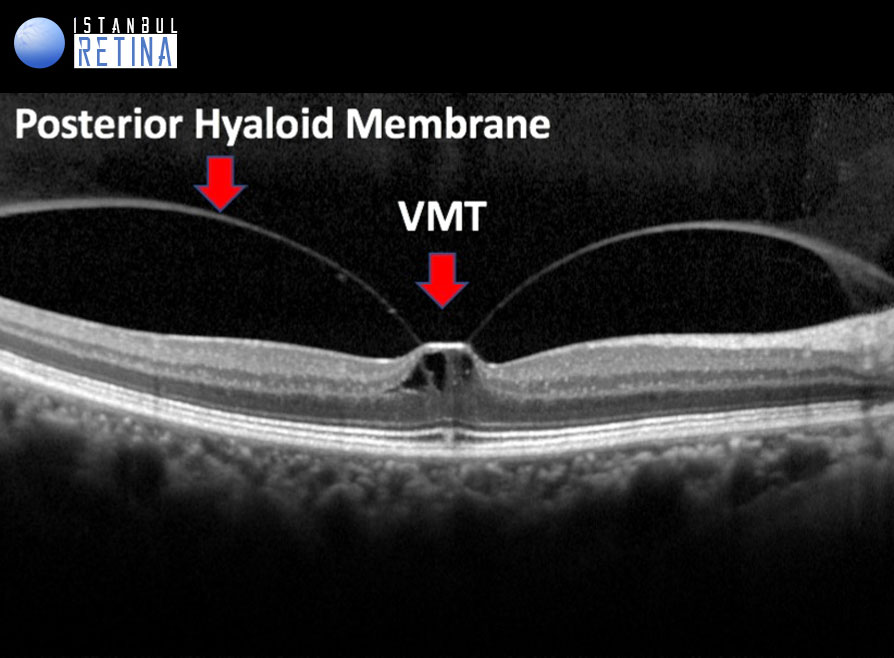
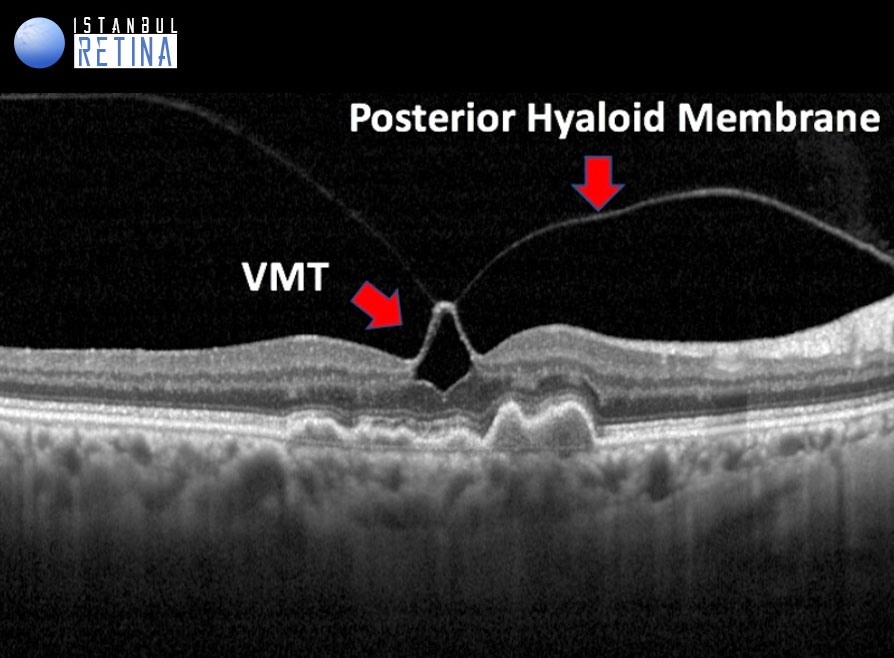
All of the following anatomic criteria must appear on at least 1 B-mode OCT scan to classify an eye as having VITREOMACULAR TRACTION: (1) evidence of perifoveal vitreous cortex detachment from the retinal surface; (2) macular attachment of the vitreous cortex within a 3-mm radius of the fovea; and (3) association of attachment with distortion of the foveal surface, intraretinal structural changes, elevation of the fovea above the RPE, or a combination thereof, but no full- thickness interruption of all retinal layers.
The pathogenesis of vitreomacular traction is thought to be caused by forces that create traction in the anteroposterior and tangential direction. Due to the size and strength of these forces, smaller areas of adhesion are expected to cause more complications.
Vitreomacular traction can be subclassified into either focal or broad, depending on the width of vitreous attachment (FOCAL (≤1500μm) or BROAD (>1500 mm). Broad areas of attachment with traction can cause generalized thickening of the macula, vascular leakage on fluorescein angiography, macular schisis, and cystoid macular edema. Focal areas of vitreous attachment with traction tend to distort the foveal surface, elevate the foveal floor, form pseudocysts within the central macula, or result in a combination thereof. The presence of pseudocysts usually is associated with diminished visual acuity and visual distortion. After release of traction, pseudocysts generally resolve over time with little remaining visual deficit.
Duker JS, Kaiser PK, Binder S, et all. The International Vitreomacular Traction Study Group Classification of Vitreomacular Adhesion, Traction, and Macular Hole. Ophthalmology 2013;120:2611-2619