Medical History:
A 16-year-male patient presented to our clinic for an annual examination.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
Best corrected visual acuity was 9/10 in the right eye and 9/10 in the left eye. Intraocular pressure was 13 mmHg in the right eye and 14 in the lefte ye. Anterior segment examination was unremarkable. Dilated funduscopic examination revealed dilated and tortuous vessels extending to the retinal periphery in the left eye (Fig. 1). Right eye was normal.
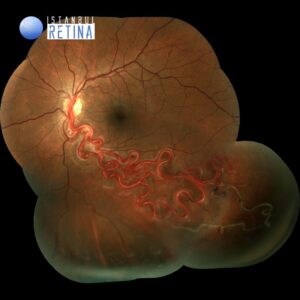
Fluorescein angiography reveales retinal arteriovenous malformations composed of dilated and tortuous vessels (Fig. 2).

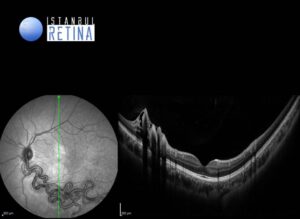
Optical coherence tomography (OCT) reveales a pattern of circular lesions corresponding to cross-sections of abnormal retinal vessels (Fig. 3).
Diagnosis
Wyburn-Mason Syndrome
Wyburn-Mason syndrome is an extremely uncommon, non-hereditary, congenital phakomatoses leading to multiple arteriovenous malformations (AVMs) that affect the eye, brain and facial structures. The exact cause of Wyburn-Mason syndrome is not known. It is proposed that it may be result of abnormal blood vessel development during embryonic or fetal growth. About 30% of the patients with the retinal lesions have brain involvement. When involving the brain, these AVM tend to localize to the midbrain region, thus necessitating neurologic imaging to rule out potentially life-threatening lesions in this area. The AVMs can affect the entire retina (30%) or be located more focally in one or more quadrants of the retina (70%). Small retinal arteriovenous malformations may cause no visual symptoms. Larger arteriovenous malformations can produce severe vision loss and are usually diagnosed in early life.
The diagnosis of Wyburn-Mason syndrome is based on its clinical presentation. The ophthalmoscopic presentation of retinal AVMs is characteristic with dilated and tortuous vessels present over the optic disc and extending variably to the retinal periphery. Fluorescein angiography may be required to demonstrate smaller lesions. OCT can also confirm the diagnosis and is very useful for the diagnosis of associated macular edema.
Differential Diagnosis
Sturge-Weber Syndrome, Von Hippel- Lindau Disease, Retinal capillary hemangioma
Treatment
The majority of retinal AVMs can remain stable over many years. Patients with neovascular glaucoma require retinal photocoagulation to treat retinal ischemia. Vitrectomy is indicated for non-clearing vitreous hemorrhage. Cyclodestructive procedures may be required in the management of refractory neovascular glaucoma. Macular edema has been successfully managed with intravitreal injection of anti-VEGF agents.
References:
- So JM, Mishra C, Holman RE. Wyburn-Mason Syndrome. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 https://www.ncbi.nlm.nih.gov/books/NBK493218/
2. Schmidt D, Pache M, Schumacher M. The congenital unilateral retinocephalic vascular malformation syndrome (bonnet-dechaume-blanc syndrome or wyburn-mason syndrome): review of the literature. Surv Ophthalmol. 2008;53(3):227-49. https://pubmed.ncbi.nlm.nih.gov/18501269/
3. Callahan AB, Skondra D, Krzystolik M, Yonekawa Y, Eliott D. Wyburn-Mason Syndrome Associated with Cutaneous Reactive Angiomatosis and Central Retinal Vein Occlusion. Ophthalmic Surg Lasers Imaging Retina. 2015;46(7):760-2. https://pubmed.ncbi.nlm.nih.gov/26247458/