Medical History:
A 60-year-old female patient presented to our clinic for an annual examination.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
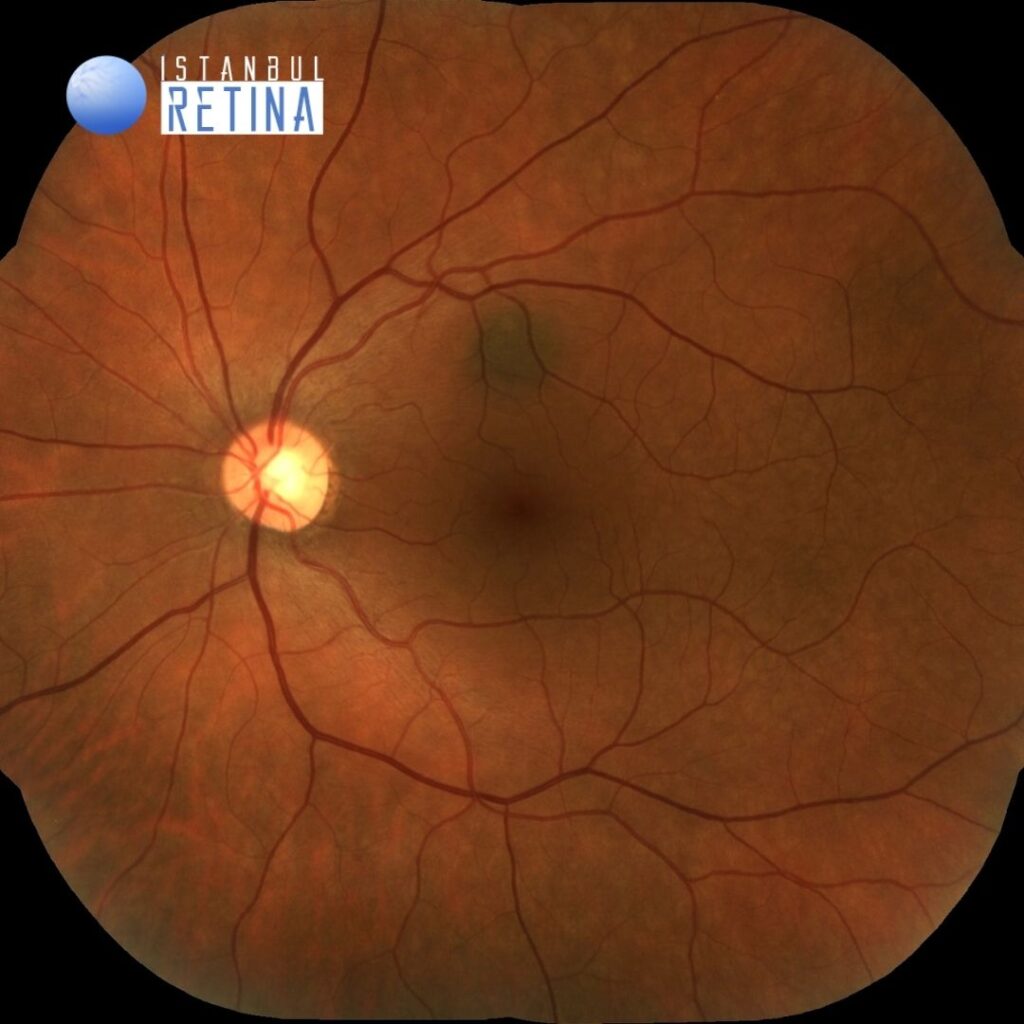
Best corrected visual acuity was 10/10 in the right eye and 10/10 in the left eye. Intraocular pressure was 17 mmHg in the right eye and 16 in the lefte ye. Anterior segment examination was unremarkable. Funduscopic examination revealed a round pigmented lesion superior to the macula in the left eye (Figure 1).
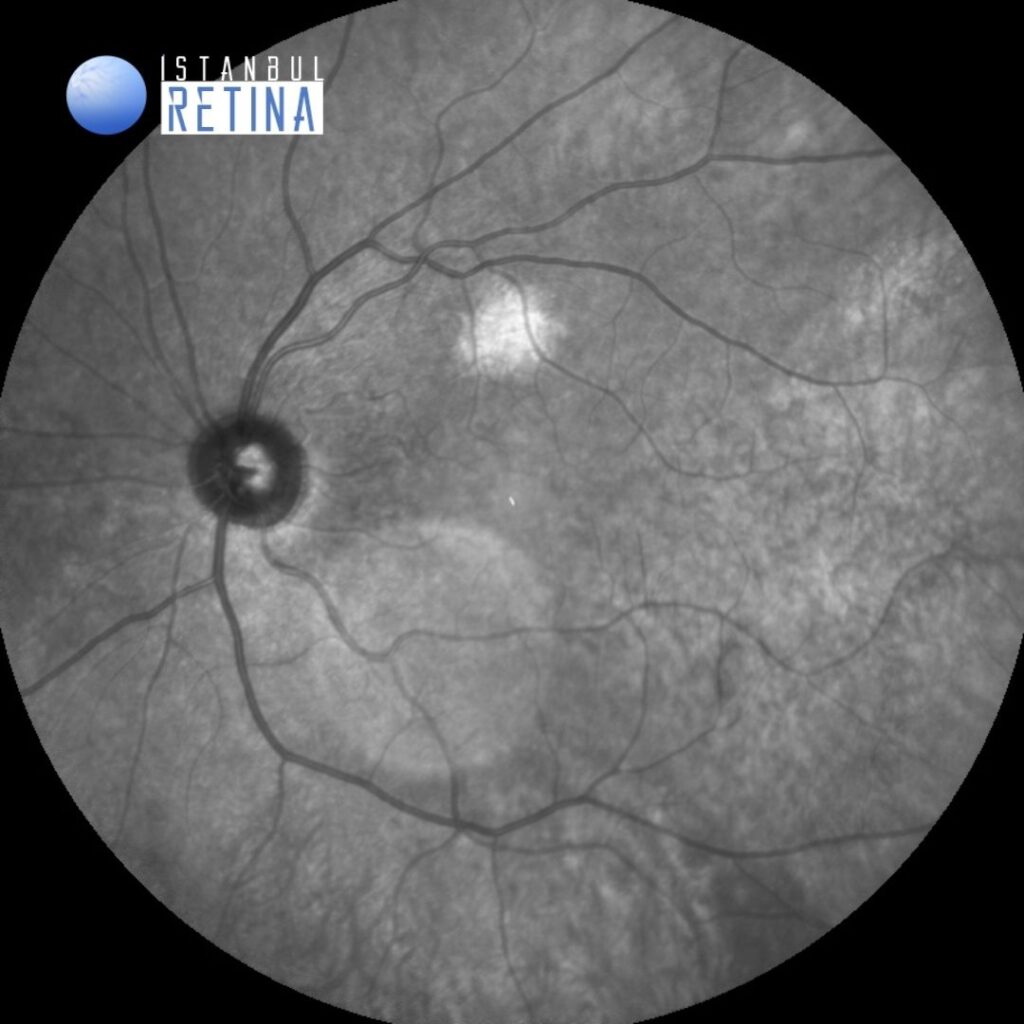
The lesion is identified on infrared reflectance image as a white patch of hyperreflectance corresponding to the choroidal nevus (Figure 2).
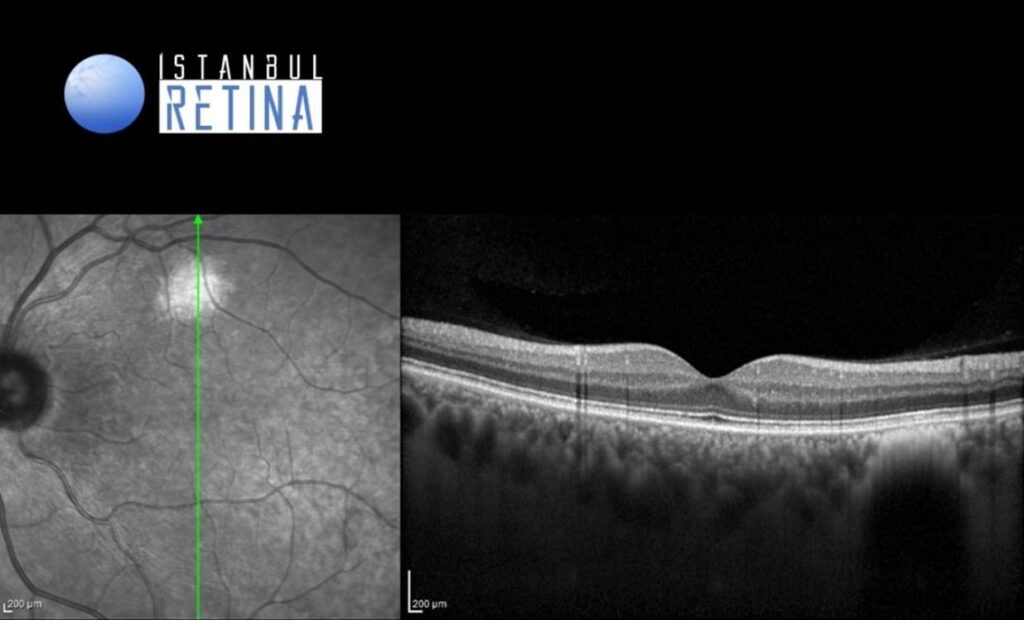
The spectral domain optical coherence tomography (OCT) scan passing through the lesion identifies the choroidal nevus as a hyperreflective lesion with posterior shadowing (Figure 3).
Diagnosis
Choroidal Nevus
The prevalence of choroidal nevus ranges from 4.6 percent to 7.9 percent. The pesence of choroidal nevus is usually not associated with any symptoms. Choroidal nevi are benign melanocytic lesions. However, about 1 in 9000 transform into melanomas. Additional diagnostic testing of larger or suspicious nevi includes optical coherence tomography (OCT), ultrasound to measure the size and thickness of elevated nevi, fluorescein angiography, indocyanine green angiography, optical coherence tomography angiography and fundus autofluorescence.
Differential Diagnosis
Choroidal melanoma, choroidal hemangioma, choroidal metastasis, choroidal granuloma
Treatment
Most nevi do not require any specific treatment. However, choroidal neovascularization associated with nevi can be treated with intravitreal injection of anti-VEGF agents.
References:
Shields JA, Shields CL. Choroidal nevus: a review of prevalence, features, genetics, risks, and outcomes. Curr Opin Ophthalmol. 2017;28:228-237. https://pubmed.ncbi.nlm.nih.gov/28141766/