Medical History:
An 85-year-old female patient presented to our clinic complaining of decreased vision.
Diabetes mellitus (+)
Systemic hypertension (+)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
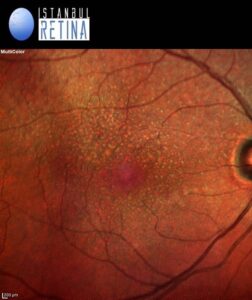
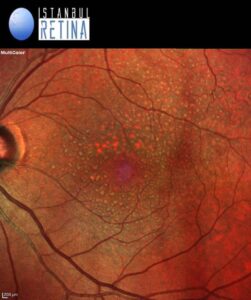
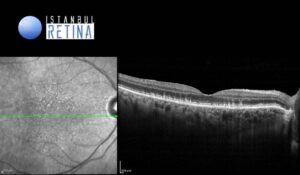
Best corrected visual acuity was 8/10 in the right eye and 8/10 in the left eye. Intraocular pressure was 16 mmHg in both eyes. Anterior segment examination revealed PC-IOL in both eyes. Funduscopic examination revealed bilateral perifoveal multiple dot like whitish-yellow deposits (Figure 1).
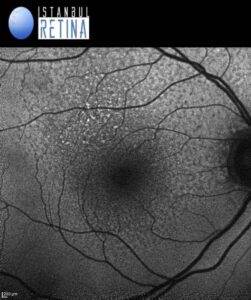
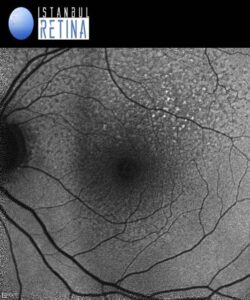
Fundus autofluorescence imaging showed numerous spots of reduced autofluorescence (Figure 2).
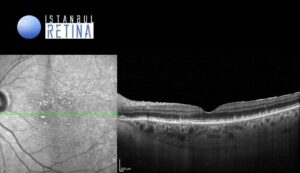
SD-OCT revealed granular hyperreflective deposits situate between the retinal pigment epithelium (RPE) layer and the ellipsoid zone (Figure 3).
Diagnosis
Reticular Pseudodrusen
Reticular drusen, also known as reticular pseudodrusen or subretinal drusenoid deposits were first described by Mimoun et al. in 1990. Arnold and colleagues named these lesions as reticular pseudodrusen. Contrary to the drusen which lie below the retinal pigment epithelium (RPE), reticular pseudo-drusen are located superficial to the RPE. Reticular pseudodrusen are identified commonly in eyes with age-related macular degeneration (AMD) and are of important prognostic value and represent a significant risk factor for the progression of AMD particularly toward conversion to late-stage AMD (complete RPE, outer retinal atrophy and macular neovascularization). Reticular pseudodrusen are not disease specific for AMD, but have also been described in association with other retinal disease entities, including Sorsby’s fundus dystrophy, pseudoxanthoma elasticum, and foveomacular vitelliform dystrophy.
OCT has been used to classify reticular pseudodrusen into 3 types by Zweifel et al.
Type 1 Hyperreflective material between RPE and inner segment-outer segment junction or ellipsoid zone (EZ). There is no elevation or breach of EZ.
Type 2 The hyperreflective material accumulates and forms a mound over the RPE with distortion of overlying EZ.
Type 3 The hyperrefelctive material has a conical configuration which punctures the EZ and reaches outer retina.
Differential Diagnosis
Cuticular drusen, macular laser spots
Treatment
Patients with reticular pseudodrusen and intermediate or advanced AMD should be followed per AREDS2 management recommendations. If macular neovascularization occurs intravitreal anti-VEGF treatment is recommended.
References:
- Arnold JJ, Sarks SH, Killingsworth MC, Sarks JP. Reticular pseudodrusen. A risk factor in age-related maculopathy. Retina. 1995;15:183–191. https://pubmed.ncbi.nlm.nih.gov/7569344/
- Domalpally A, Agrón E, Pak JW, et al. Prevalence, Risk, and Genetic Association of Reticular Pseudodrusen in Age-related Macular Degeneration: Age-Related Eye Disease Study 2 Report 21. Ophthalmology. 2019;126:1659–1666. https://pubmed.ncbi.nlm.nih.gov/31558345/
- Holz FG, Saßmannshausen M. Reticular Pseudodrusen: Detecting a Common High-Risk Feature in Age-Related Macular Degeneration. Ophthalmol Retina. 2021;5(8):719-720. https://pubmed.ncbi.nlm.nih.gov/34364530/


