Medical History:
A 45-year-old male patient presented with complaint of blurry vision in both eyes for the past 3 years.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
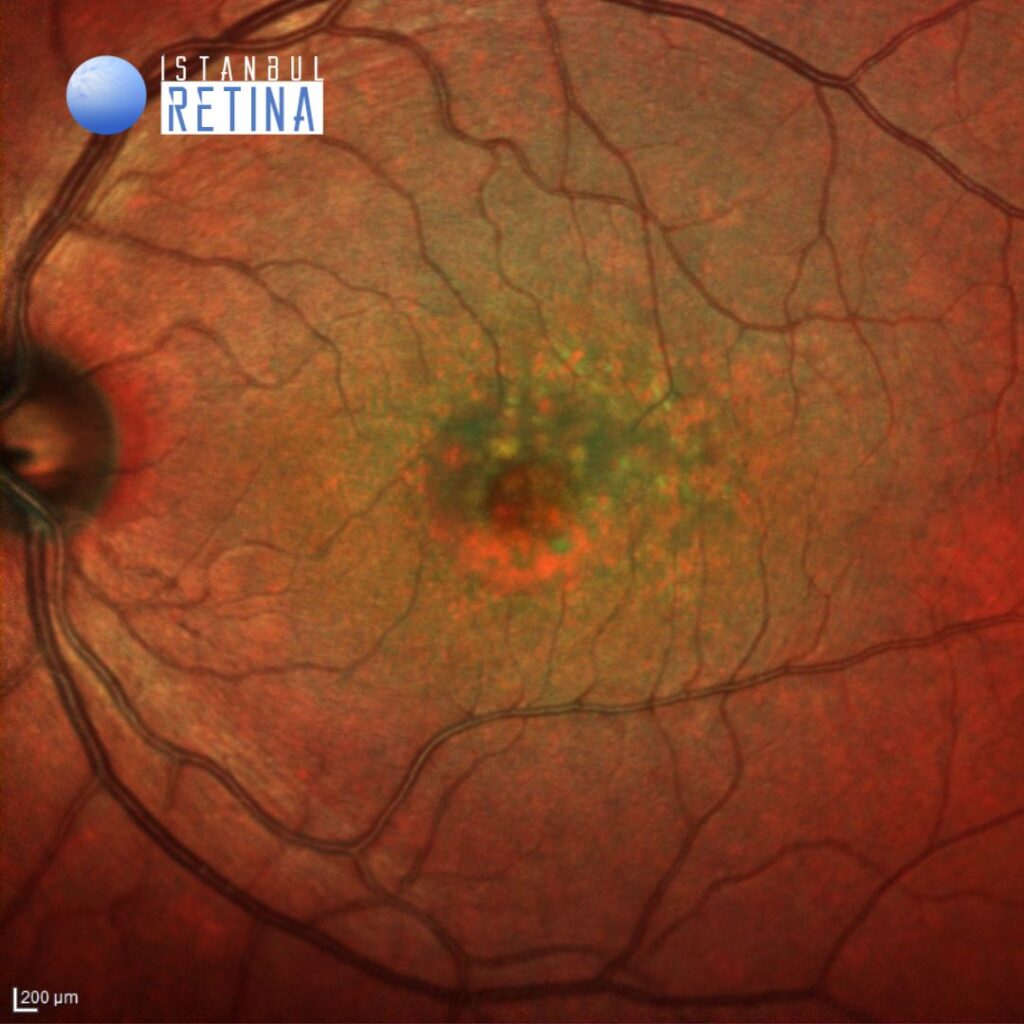
Best corrected visual acuity was 7/10 in the right eye and 7/10 in the left eye. Intraocular pressure was 12 mmHg in both eyes. Anterior segment examination was unremarkable. Funduscopic examination revealed roundish yellow lesions, clustering in the macular region and vitelliform lesion under the fovea in both eyes (Figure 1).
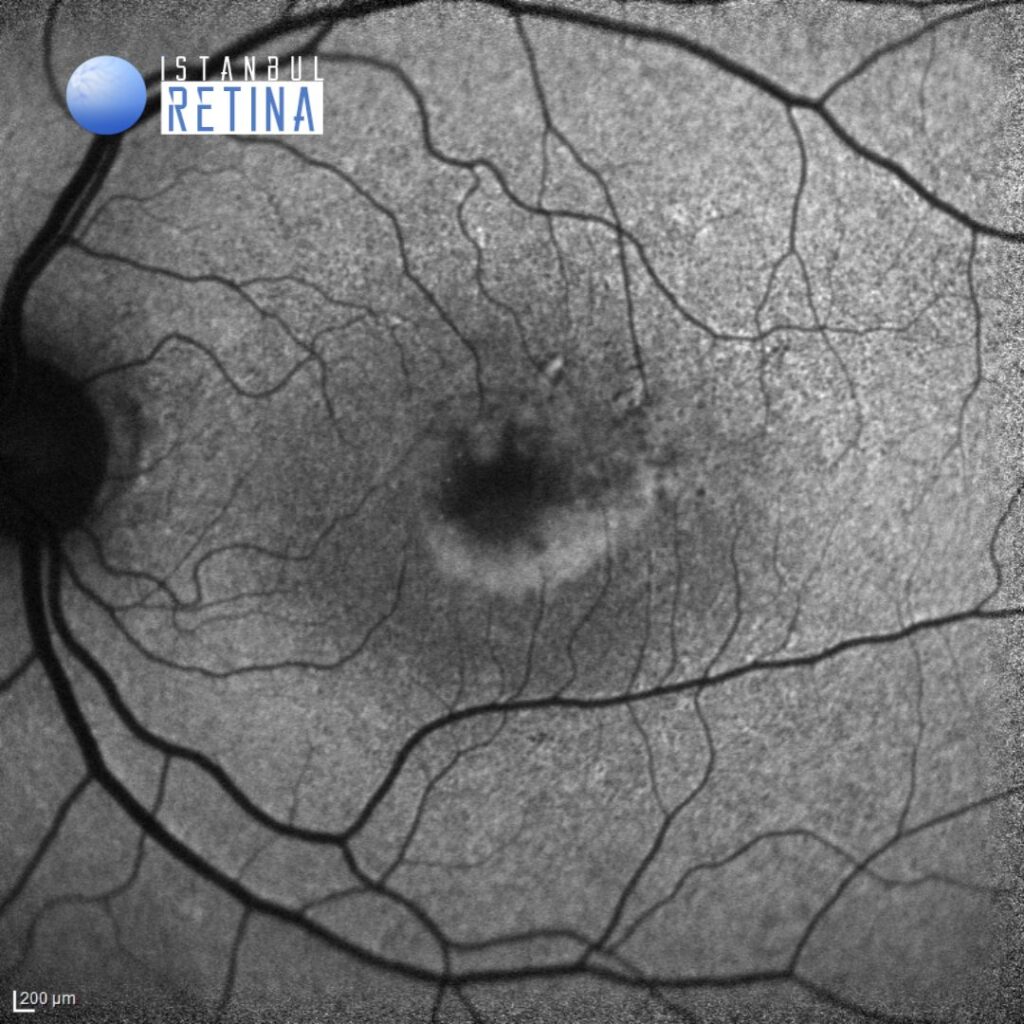
Fundus autofluorescence imaging shows central hypoautofluorescence surrounded by a ring of hyperfluorescence (Figure 2).
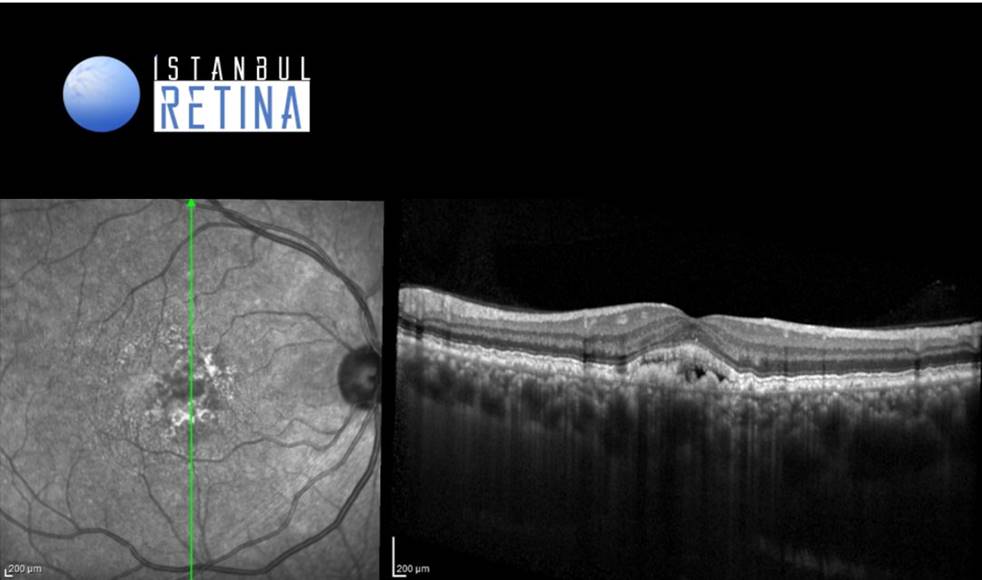
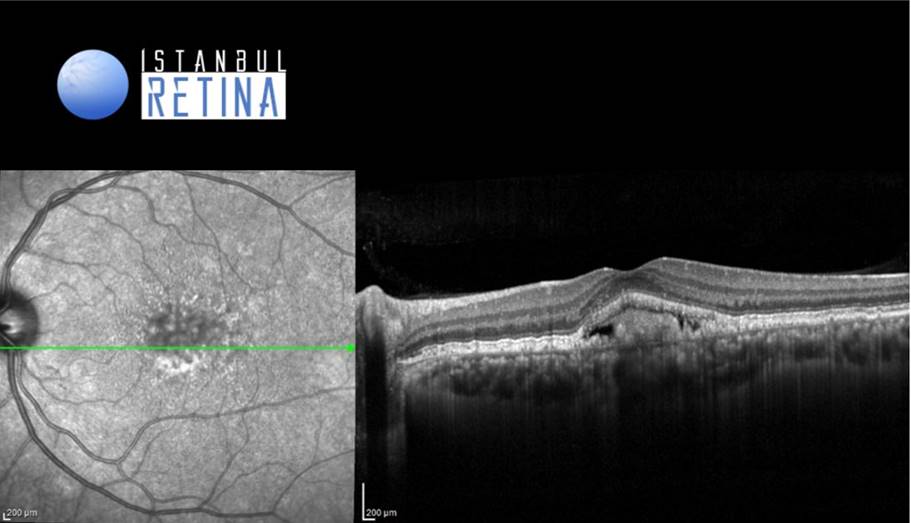
Optical coherence tomography (OCT) shows discrete retinal pigment epithelium (RPE) elevations compatible with cuticular drusen and accumulation of hyperreflective subretinal material with an overlying hyporeflective space (Figure 3).
Diagnosis
Vitelliform Macular Lesion Associated with Cuticular Drusen
The clinical entity of cuticular drusen was first described in 1985 by Gass. Cuticular drusen share with conventional drusen the localization between RPE-basal lamina and Bruch’s membrane. Although sharing a similar content with hard drusen, cuticular drusen are numerous and tend to coalescence.
Cuticular drusen appear clinically as a myriad of roundish yellow lesions, clustering in the macular region and/or mid-peripheral retina. They typically measure between 50 and 75 μm in diameter. The typical appearance of cuticular drusen is represented by the “starry-sky” pattern characterized by several roundish hyperfluorescent lesions during the arteriovenous phase of fluorescein angiography. On OCT scans, cuticular drusen demonstrate triangular elevations of the retinal pigment epithelium, conferring a characteristic “saw-tooth” pattern.
One of the first clinical associations described for cuticular drusen was the vitelliform macular lesion. Patients with the combination of vitelliform macular detachment and cuticular drusen were younger and presented with worse visual acuity when compared with adult-onset vitelliform macular dystrophy. The prevalence of acquired vitelliform lesions in patients with cuticular drusen varied by ethnic group from 1.2% in the Asian population to 24.2% in Caucasians. The vitelliform macular detachment on OCT appears as hyperreflective subretinal material with an overlying hyporeflective space. The fate of vitelliform detachment associated with cuticular drusen includes collapse with resolution of the vitelliform material and accompaniment of progressive RPE failure and atrophy with drusen disappearance. Moreover, the lesions may lead to development of macular neovascularization (MNV) among 30% of cases.
Differential Diagnosis
Autosomal dominant drusen (Malattia Leventinese), pattern macular dystrophy, North Carolina macular dystrophy, Sorsby macular dystrophy, adult vitelliform foveomacular dystrophy
Treatment
In cases of isolated cuticular drusen or vitelliform macular detachments associated with cuticular drusen, no therapy is indicated. There have been reports of improvement in vision in MNV patients with cuticular drusen through the use of bevacizumab injections.
References:
Fragiotta S, Fernández-Avellaneda P, Breazzano MP, Scuderi G. Clinical Manifestations of Cuticular Drusen: Current Perspectives. Clin Ophthalmol. 2021;15:3877-3887.