Medical History:
A 41-year-old male patient presented with complaint of sudden painless loss of vision in the left eye after performing a Valsalva-type maneuver.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
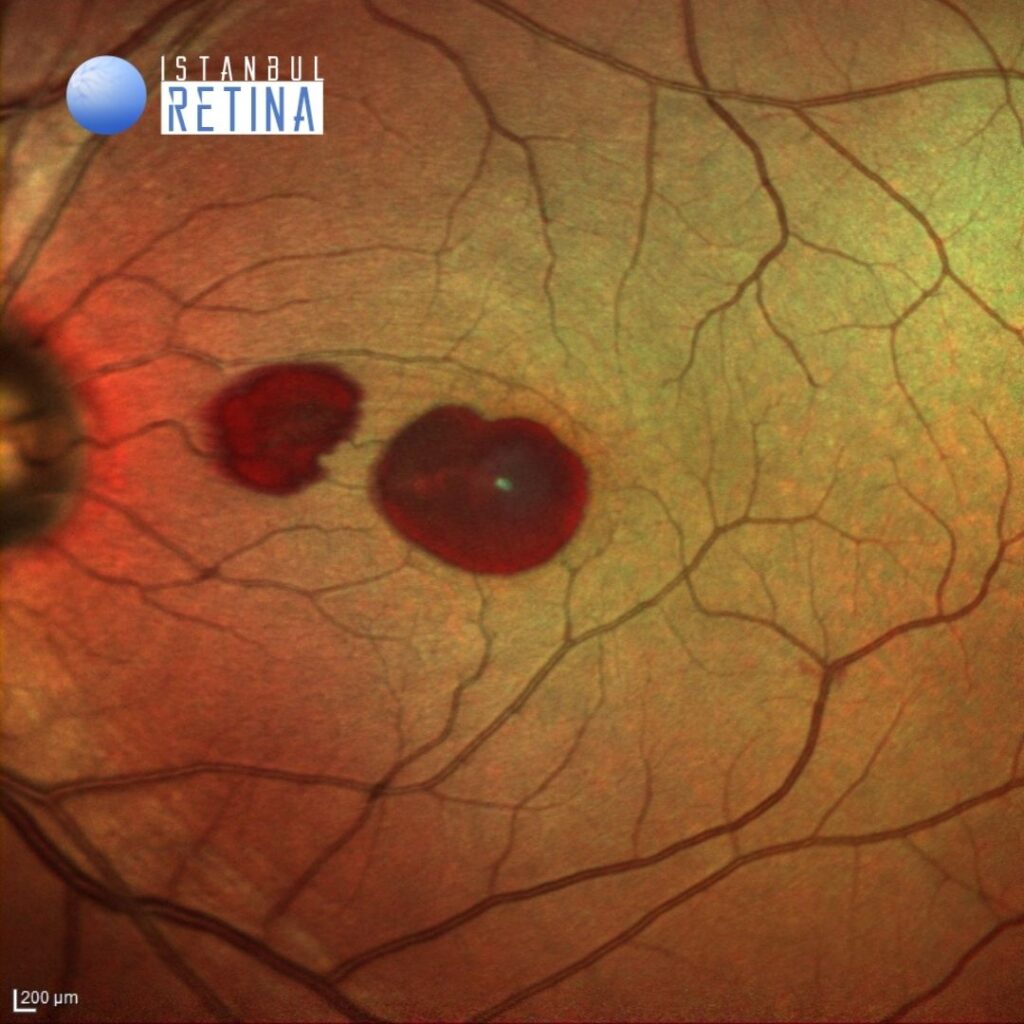
Best corrected visual acuity was 10/10 in the right eye and 1/10 in the left eye. Intraocular pressure was 11 mmHg in both eyes. Anterior segment examination was unremarkable. Funduscopic examination revealed well-circumscribed and oval shaped premacular hemorrhages in the left eye (Figure 1). Fundus examination of the right eye was normal.
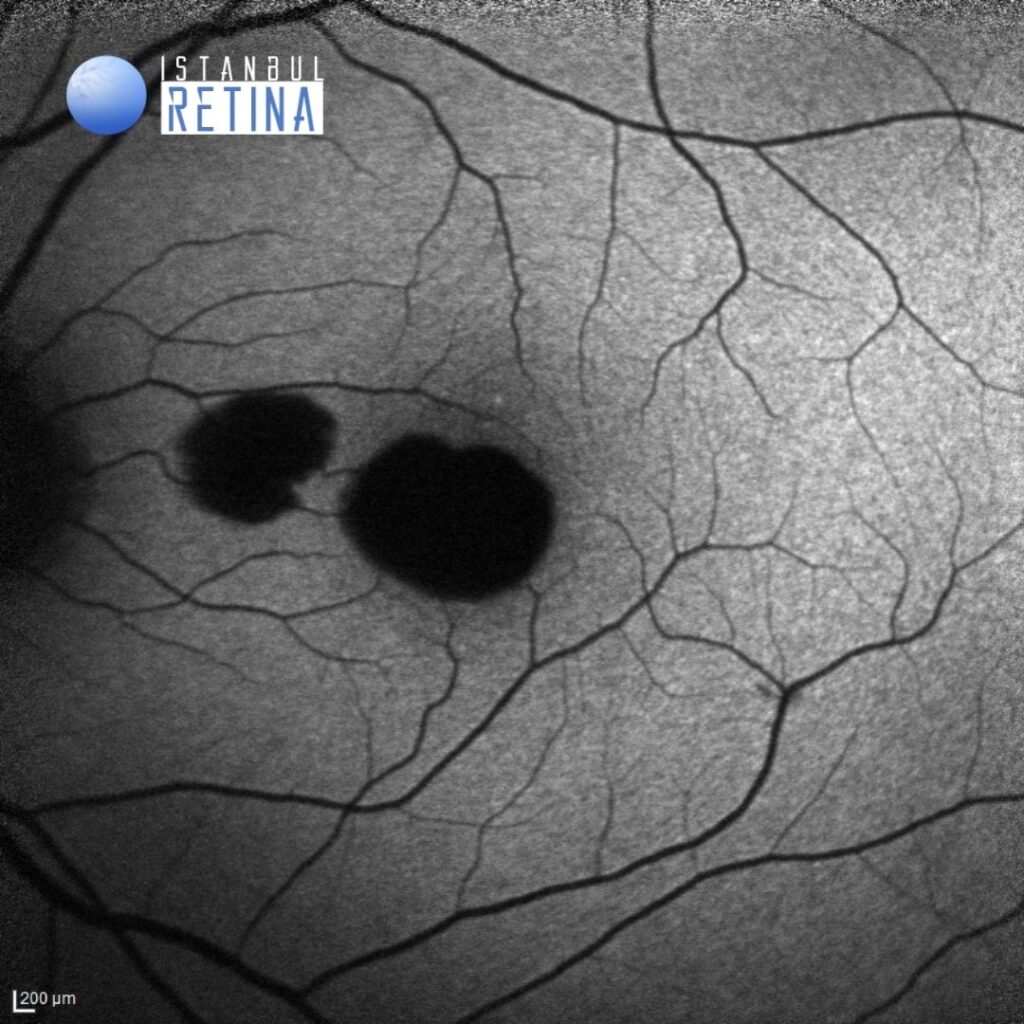
Fundus autofluorescence demonstrated marked hypoautofluorescence in the areas of hemorrhage (Figure 2).
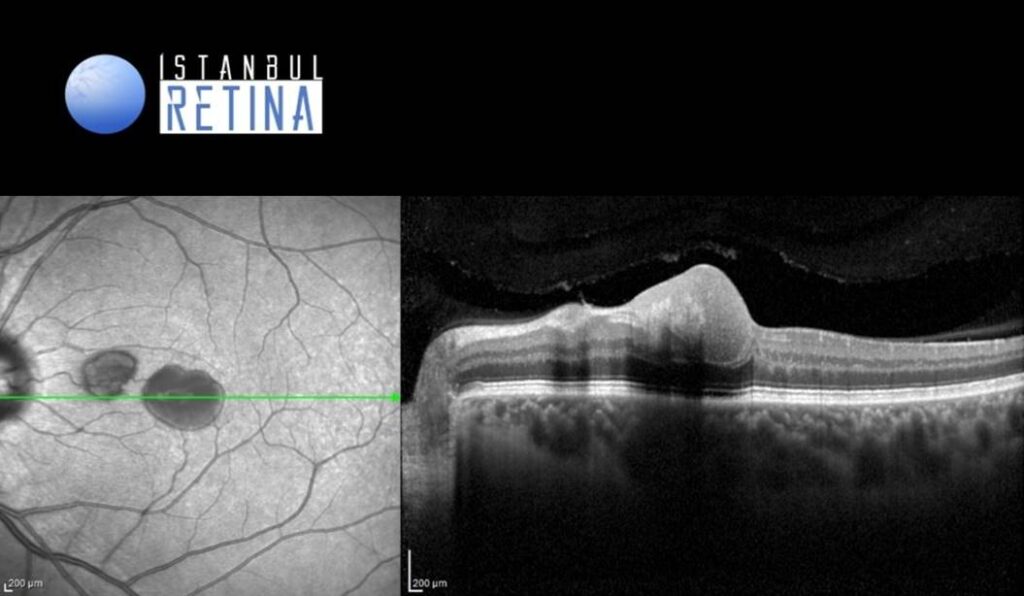
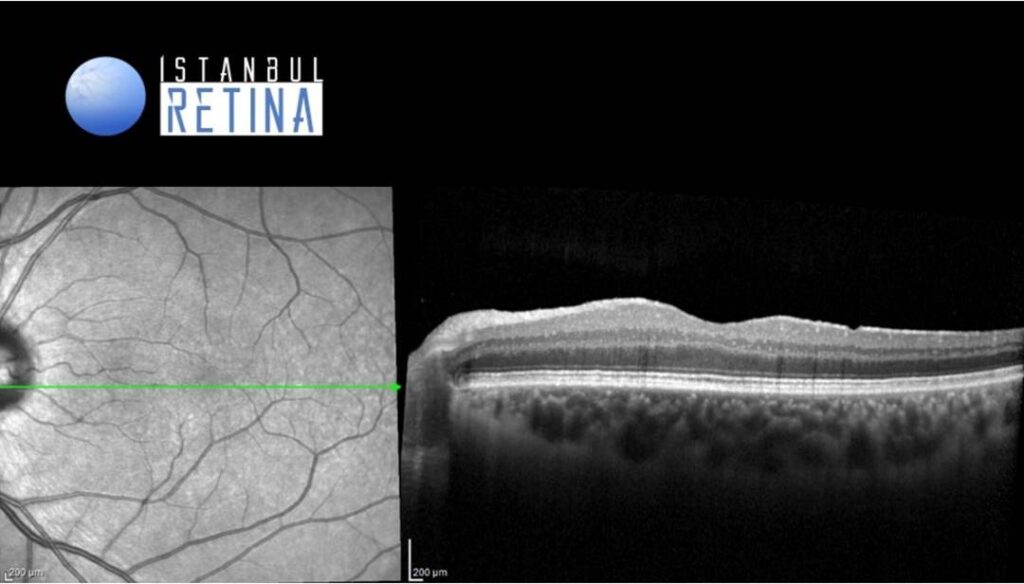
SD-OCT showed a dense hyperreflective material (blood) located beneath the subhyaloid and sub-internal limiting membrane (Figure 3).
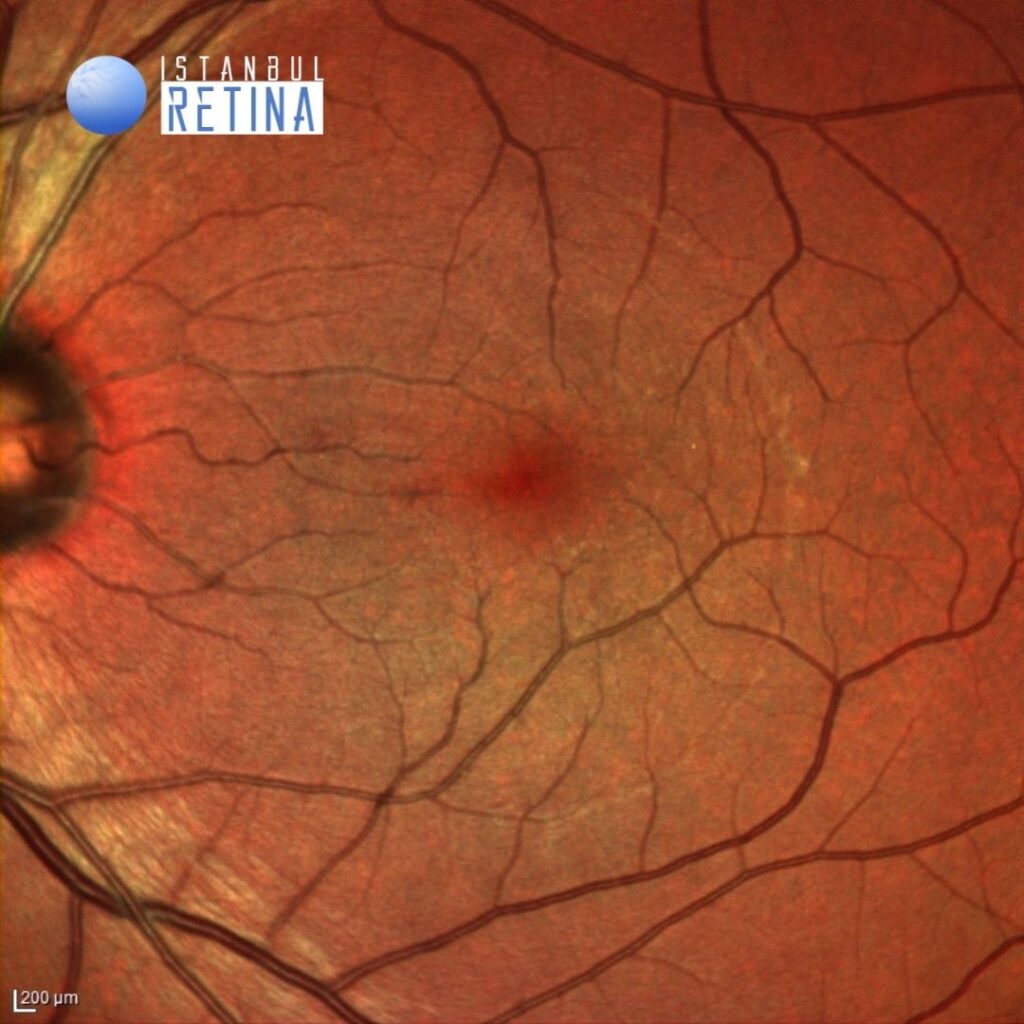
Pars plana vitrectomy with dissection of the posterior hyaloid, ILM peeling and removal of the sub-ILM hemorrhage was performed. Post-operative visual acuity after 1 month was 9/10 (Figure 4 and Figure 5).
Diagnosis
Valsalva Retinopathy
Valsalva retinopathy is a specific form of retinopathy characterized by pre-retinal hemorrhage secondary to raised intrathoracic pressure (valsalva maneuver). Valsalva maneuver includes: weight lifting, vomiting, coughing, sneezing, aerobic exercises, constipation, blowing musical instruments, straining, physical activities, sexual intercourse and compression injuries. Patients present with sudden onset painless painless vision loss. The sudden rise of intraocular venous pressure leads to rupture of perifoveal superficial retinal capillaries causing pre-retinal hemorrhage, either beneath the sub internal limiting membrane or subhyaloid space.
Differential Diagnosis
Hypertensive retinopathy, sickle cell anemia, shaken baby syndrome, Terson syndrome, ruptured macroaneurysm, anemic retinopathy, acute posterior vitreous detachment
Treatment
Treatment depends on the location of the hemorrhage. Observation is the standard treatment. However, cases of massive bleed at the macula may require early intervention. For large subhyaloid hemorrhage/sub internal limiting membrane hemorrhage obscuring macula, Nd:YAG laser membranotomy can be used to make an opening in the posterior hyaloid or ILM, so that blood escapes into the vitreous cavity and settles inferiorly. If there is significant and long-standing premacular hemorrhage, or dense vitreous hemorrhage obscuring retinal evaluation, then pars plana vitrectomy can be attempted.
References:
1.Simakurthy S, Tripathy K. Valsalva Retinopathy. [Updated 2022 Feb 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 https://www.ncbi.nlm.nih.gov/books/NBK545219/