Medical History:
A 44-year-old male patient with progressive vision loss in the right eye was examined in our clinic.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
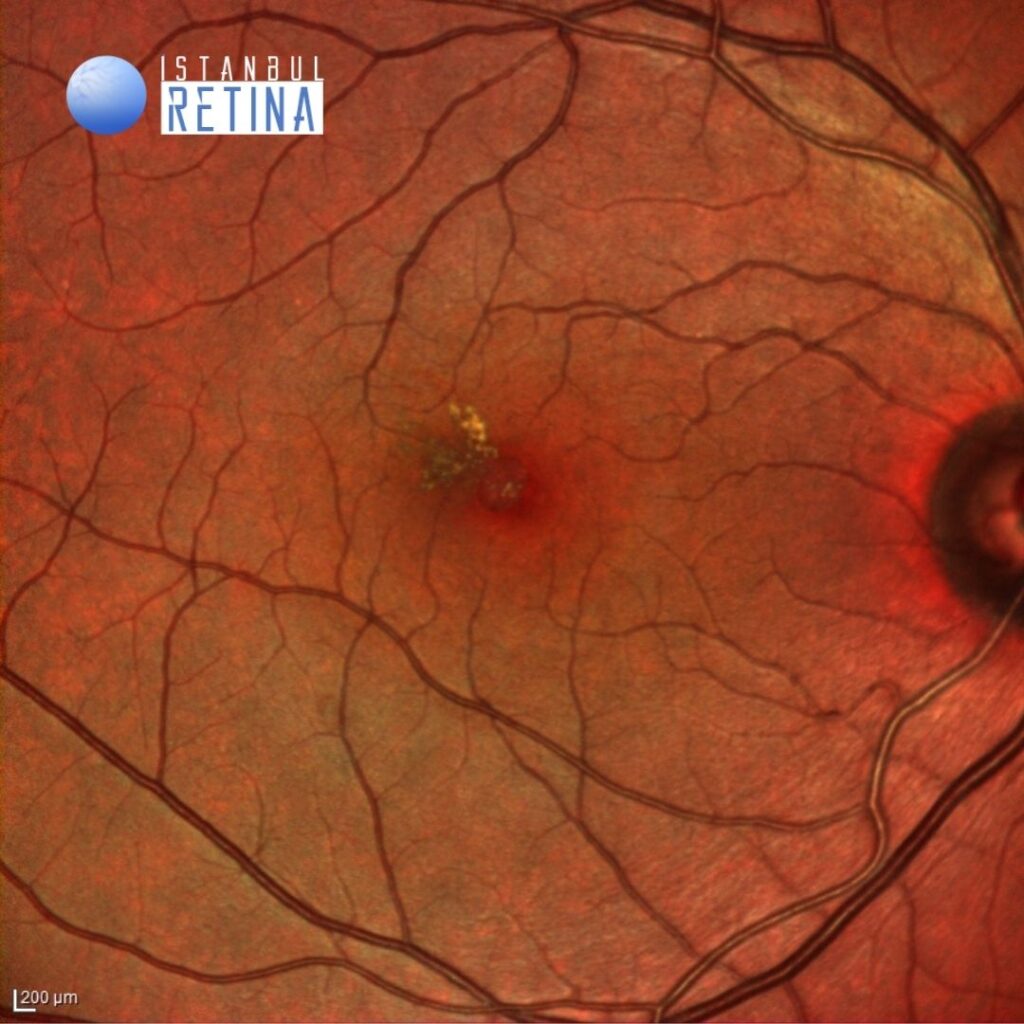
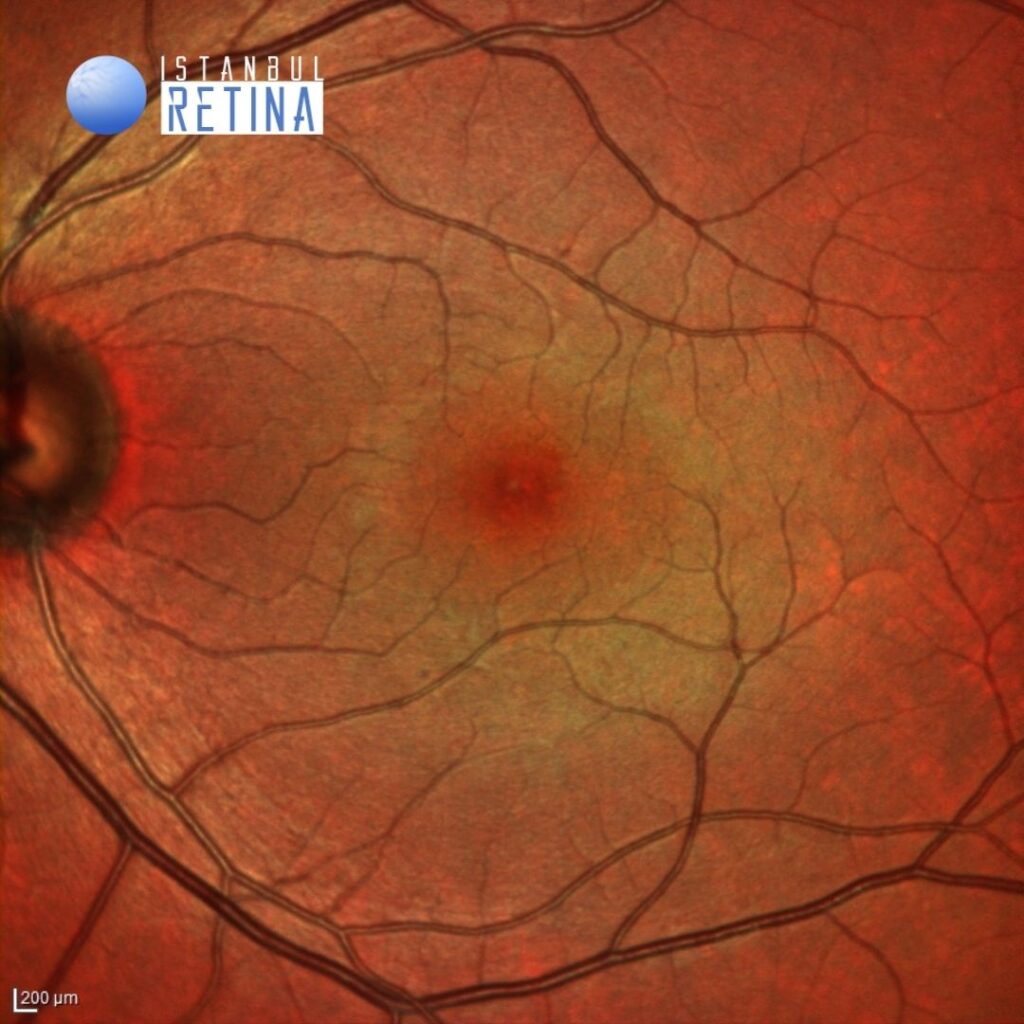
Best corrected visual acuity was 5/10 in the right eye and 10/10 in the left eye. Intraocular pressure was 14 mmHg in both eyes. Anterior segment examination was unremarkable. Funduscopic examination revealed some hard lipid exudates located temporal to the fovea in the right eye. Fundus appearance was normal in the left eye (Figure 1).
Fundus autofluorescence revealed central hyperatofluorescance and hypoautofluorescence in the area of lipid exudates in the right eye and normal fundus autofluorescence in the left eye (Figure 2).
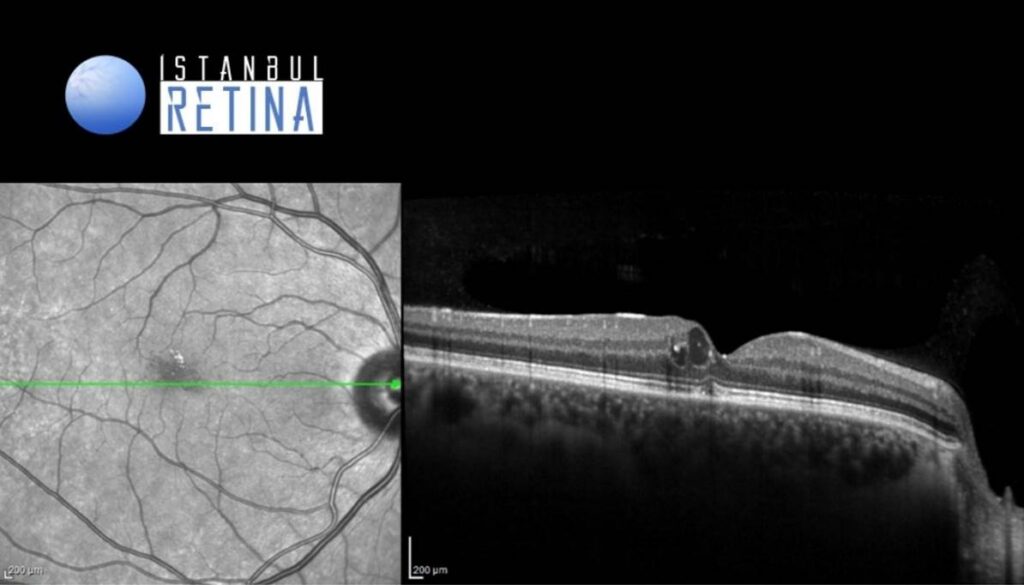
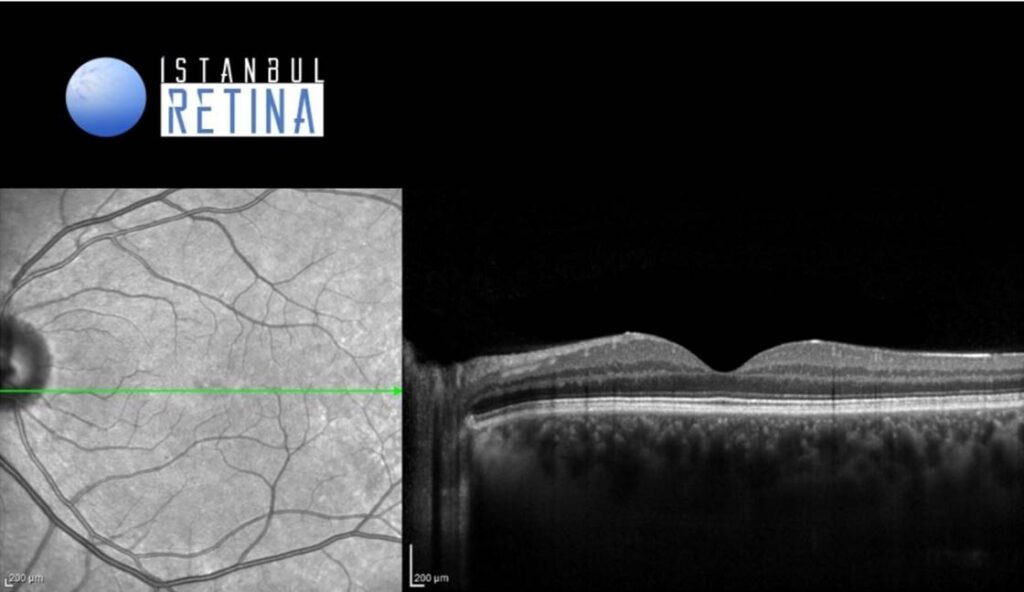
SD-OCT showed intraretinal cysts located temporal to the fovea in the right eye. Normal OCT findings were observed in the left eye (Figure 3)
Diagnosis
Macular Telangiectasia (MacTel) Type 1
Macular telangiectasias, often called MacTel, are characterized by retinal capillary vessel dilation affecting the macular region. There are two main groups. Type 1 MacTel (aneurysmal telangiectasia) is typically unilateral and predominantly occurs in middle-aged men. Type 2 (perifoveal telangiectasia) is more common, typically bilateral, and occurs in men and women. Type 1 MacTel, is believed to be a rare variation of Coats Disease. In Type 1 MacTel cases telangiectasias are typically involving the two disc diameter area temporal to the fovea. Macular edema, and hard exudation are the main causes of vision loss.
Differential Diagnosis
Diabetic retinopathy, macular branch retinal vein occlusion macular, age-related macular degeneration
Treatment
There is no established treatment for type 1 MacTel. Although laser photocoagulation, sub-Tenon’s capsule injection of triamcinolone acetonide, dexamethasone intravitreal implant, and intravitreal anti–vascular endothelial growth factor have been proposed as potentially effective treatment procedures.
References:
1. Yannuzzi LA, Bardal AM, Freund KB, et al. Idiopathic macular telangiectasia. Arch Ophthalmol 2006;124:450–460. https://pubmed.ncbi.nlm.nih.gov/16606869/
2. Osaka R, Shiragami C, Ono A, et al. Clinical features of treated and untreated type 1 idiopathıc macular telangiectasia without the occurrence of secondary choroidal neovascularization followed for 2 years in japanese patients. Retina. 2018 Jan;38 Suppl 1(Suppl 1):S114-S122. https://pubmed.ncbi.nlm.nih.gov/28541960/