Medical History:
A 17-year-old male patient with progressive vision loss in both eyes was examined in our clinic.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
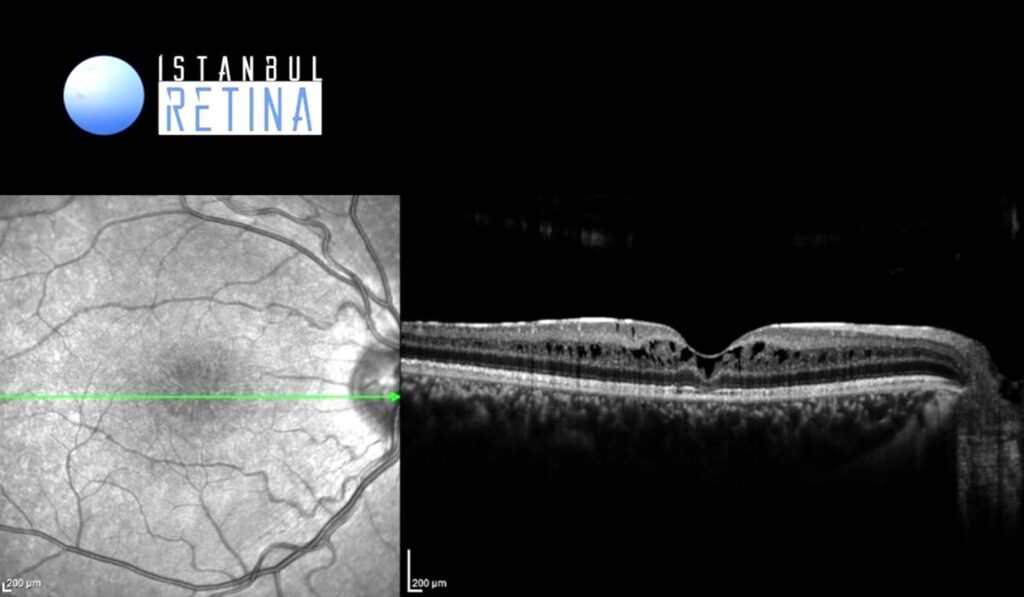
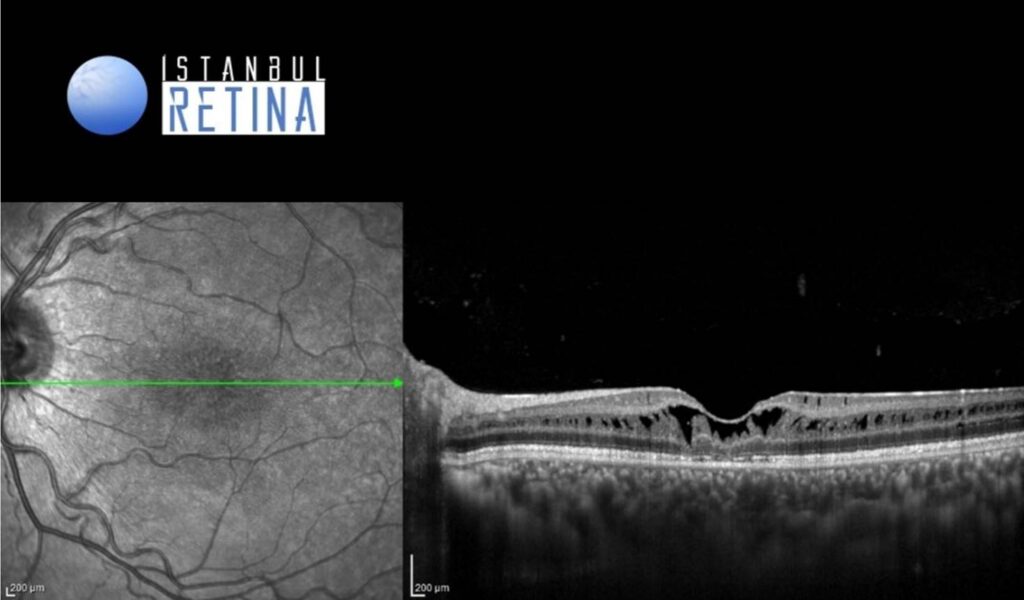
Best corrected visual acuity was 4/10 in both eyes. Intraocular pressure was 16 mmHg in both eyes. Anterior segment examination was unremarkable. Funduscopic examination revealed a spoke wheel pattern radiating from the fovea.
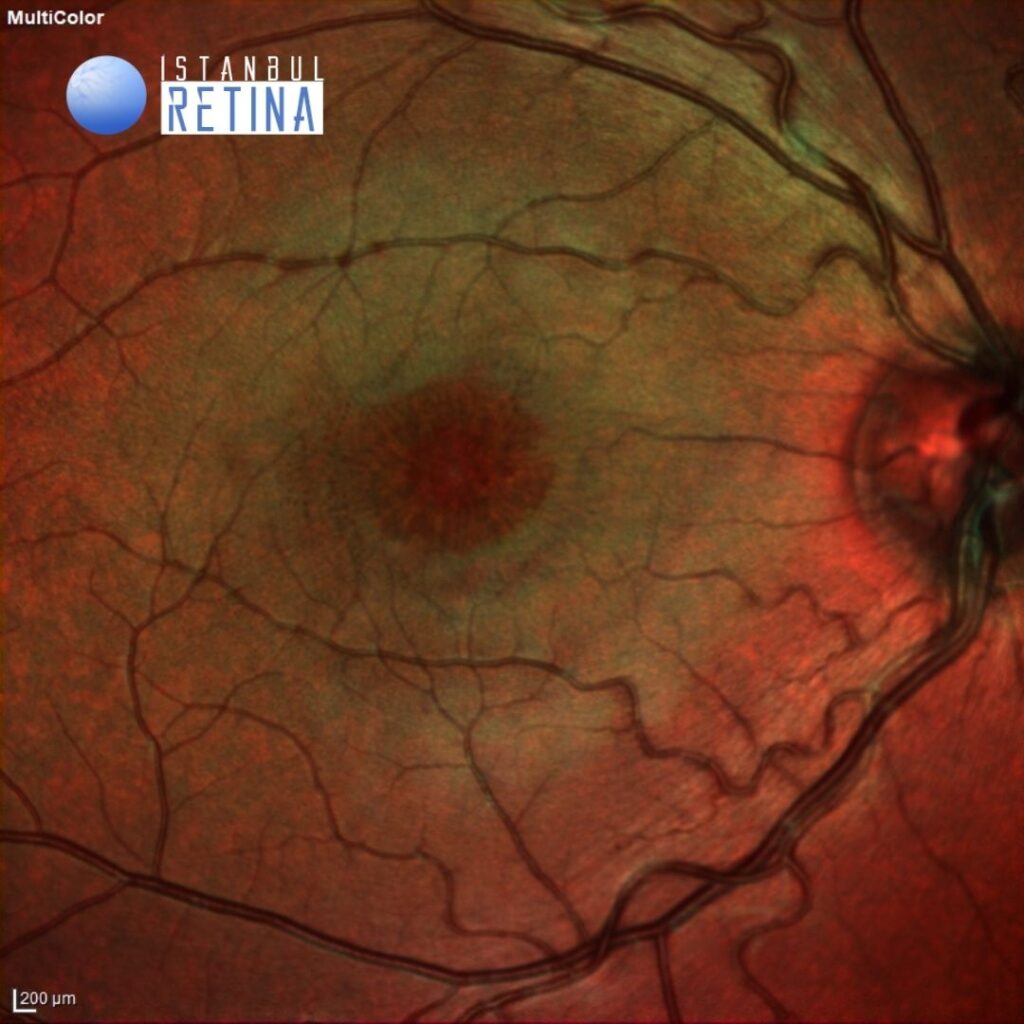
The multicolor image reveals a spoke wheel pattern radiating from the fovea (Figure 1).
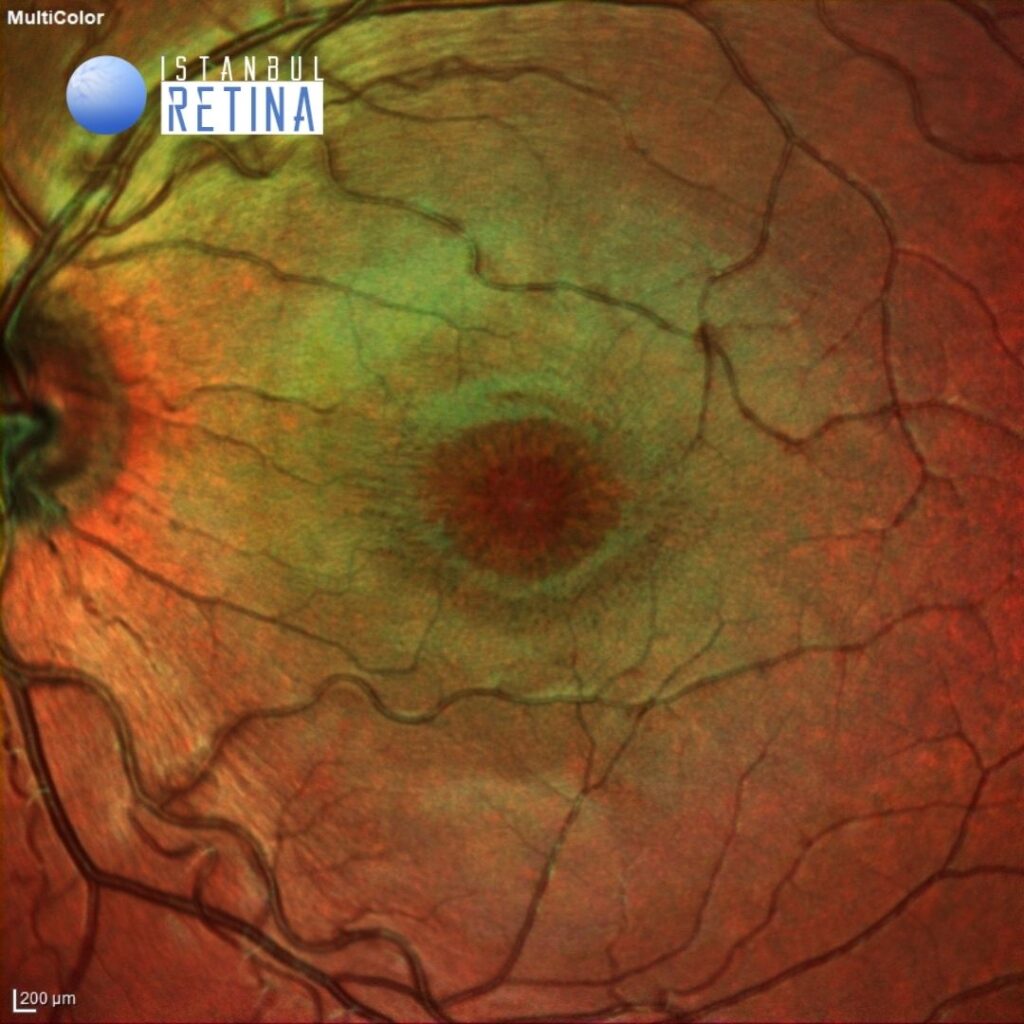
Infrared reflectance images from the same patient (Figure 2).
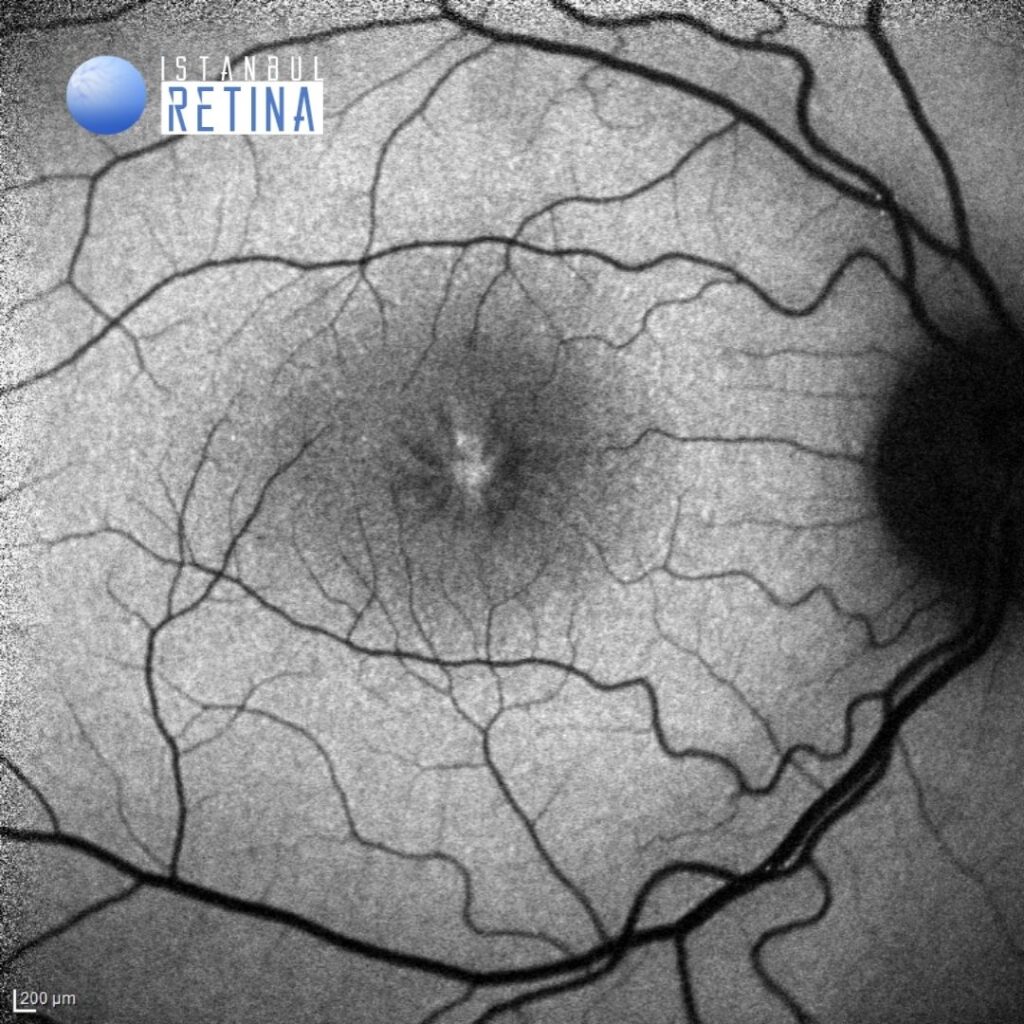
Fundus autofluorescence imaging shows a spoke wheel pattern (Figure 3).
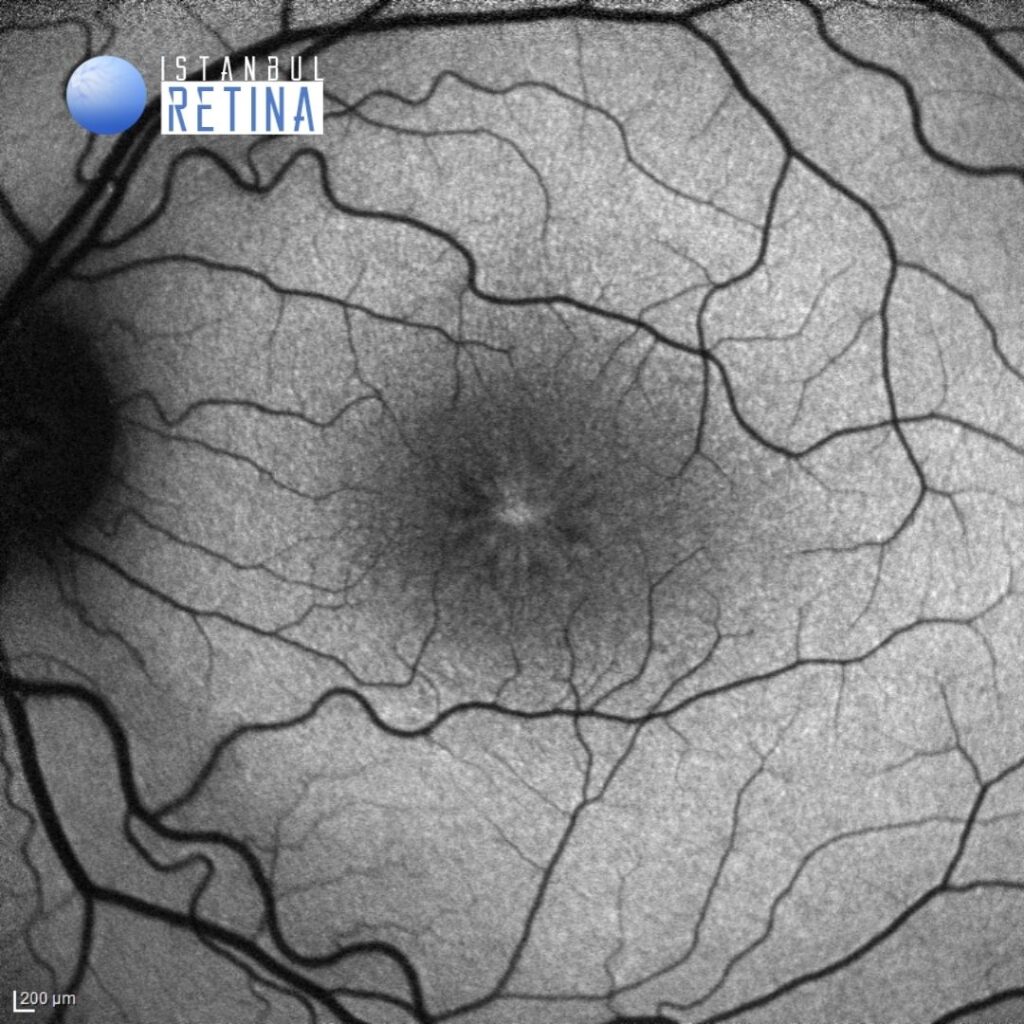
SD-OCT imaging shows marked retinoschisis in different retinal layers (Figure 4).
Diagnosis
Juvenile Retinoschisis
Juvenile retinoschisis, or X-linked retinoschisis is a rare congenital disease of the retina caused by mutations in the RS1 gene. The RS1 gene encodes retinoschisin, a protein involved in intercellular adhesion. Juvenile retinoschisis has a prevalence of about 1 in 15,000 to 30,000. It is inherited in an X-linked manner and is characterized by symmetric bilateral macular involvement beginning in the first decade of life. Most affected individuals are males, as heterozygous females are rarely affected. On fundoscopic examination, the patients have foveal schisis, noted as a spoke wheel pattern radiating from the fovea. Peripheral retinoschisis is found in 50% of the patients, most commonly in the inferotemporal quadrant.
Recently, juvenile retinoschisis has been classified into 4 phenotypes based on examination and optical coherence tomography (OCT) characteristics: type 1, foveal; type 2, foveolamellar; type 3, complex; and type 4, foveoperipheral. Foveal schisis is defined as schisis that is appreciated on clinical exam. The corresponding schisis noted on OCT does not extend beyond what is observed clinically. On the other hand, lamellar schisis is recognized on OCT as macular schisis in areas that appear normal on clinical exam.
Differential Diagnosis
Autosomal dominant and recessive schisis, Goldmann-Favre syndrome, dominant cystoid macular dystrophy
Treatment
Currently there is no approved treatment for juvenile retinoschisis.
References:
1. American Academy of Ophthalmology. X-linked juvenil retinoschisis. https://www.aao.org/image/x-linked-juvenile-retinoschisis Accessed May 20, 2020. https://www.aao.org/image/x-linked-juvenile-retinoschisis
2. Rao P, Dedania VS, Drenser KA. Congenital X-Linked Retinoschisis: An Updated Clinical Review. Asia Pac J Ophthalmol (Phila) 2018;7:169-175. https://pubmed.ncbi.nlm.nih.gov/29633586/
3. Prenner JL, Capone A Jr, Ciaccia S, et al. Congenital X-linked retinoschisis classification system. Retina 2006;26:61-64. https://pubmed.ncbi.nlm.nih.gov/16946682/