Medical History:
A 9-year-old female patient without any complaints was admitted to our clinic. Her family stated that a lesion was detected in the right eye during the annual examination performed in another medical institution.
Family history (-)
Parental consanguineous marriages (-)
Trauma (-)
Examination Findings
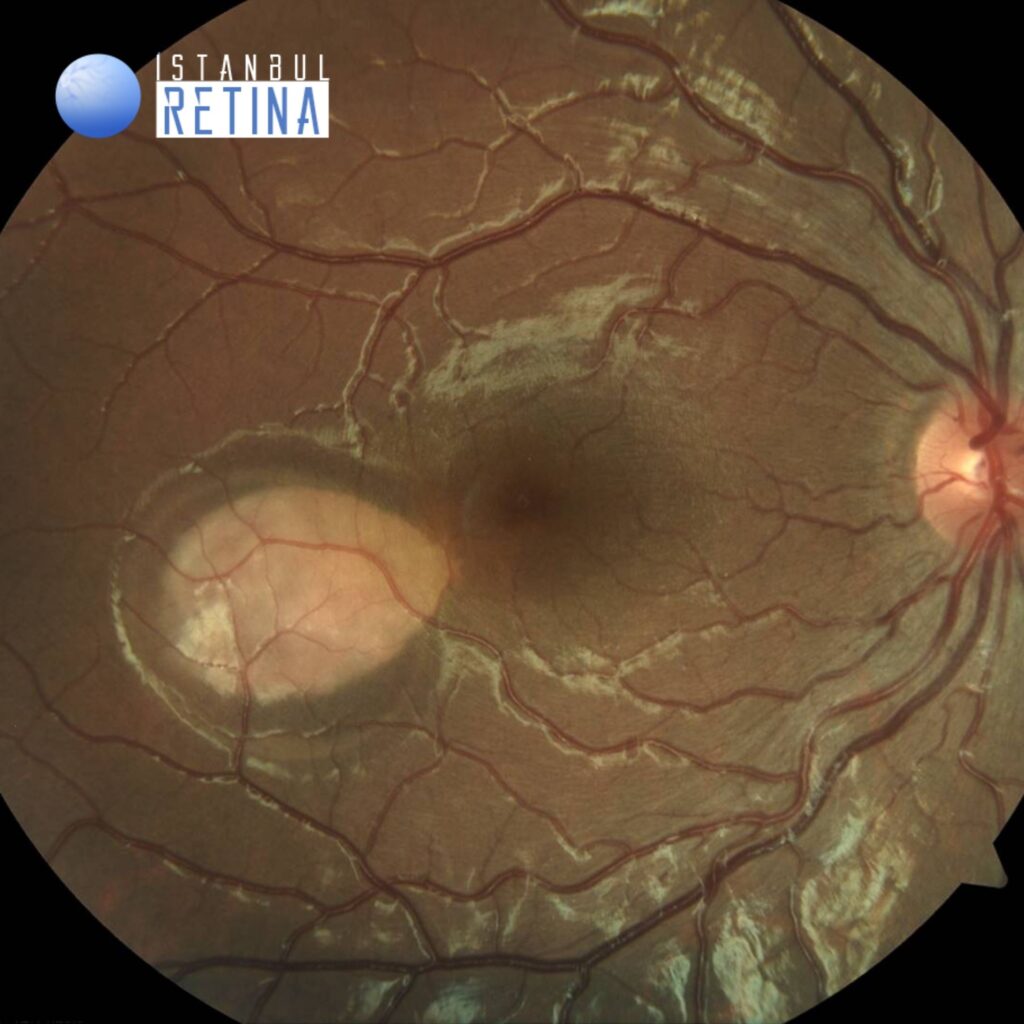
The best-corrected visual acuity was 10/10 both eyes. Intraocular pressure was 16 mmHg in both eyes. Anterior segment examination findings were normal in both eyes. Fundus examination revealed a torpedo-shaped, hypopigmented lesion temporal to the fovea of the right eye. Fundus findings were normal in the left eye.
Color fundus image of the right eye shows a torpedo-shaped, hypopigmented lesion temporal to the fovea (Figure 1).
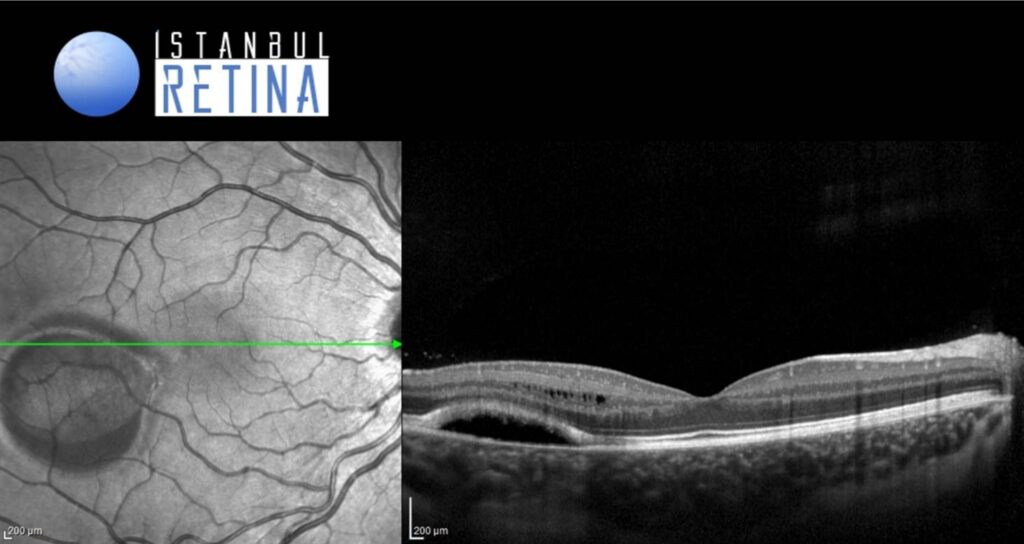
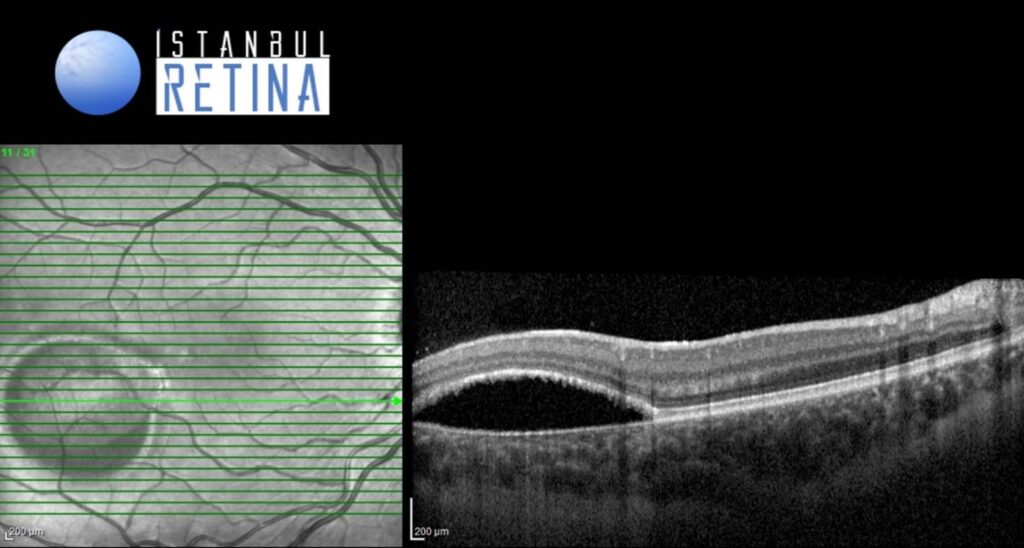
Infrared reflectance image of the same patient (Figure 2).
SD-OCT imaging revealed intraretinal cystoid spaces, ellipsoid zone thickening, and cleft between the ellipsoid zone and thinned retinal pigment epithelium (Figure 3 and Figure 4).
Diagnosis
Torpedo Maculopathy
It was first described by Roseman and Gass in 1992 as a rare and congenital anomaly of the retinal pigment epithelium. Several theories for its pathogenesis have been proposed. A developmental anomaly in the nerve fiber layer, abnormal choroidal or ciliary vessel development, persistent developmental defect in the RPE, or scarring of intrauterine chorioretinitis are a few of these theories. It is usually detected as an incidental finding during a routine eye exam. If the fovea is spared, patients are usually asymptomatic. Central scotoma is seen in cases where the fovea is affected.
In 2015, Wong et al. proposed a classification of torpedo maculopathy into two types according to the pattern of abnormality in OCT. Type 1 include lesions that show attenuation of interdigitation zone and ellipsoids, without outer retinal cavitation. Type 2 show loss of ellipsoids and interdigitation zone as well as thinning of outer nuclear layer associated with cavitation. Recently, it has been reported a Type 3 lesion, defined by excavated inner layers, retinal thinning, inner retinal hypereflective spaces, and no subretinal cleft.
Differential Diagnosis
Congenital RPE hypertrophy, RPE hamartoma, amelanotic choroidal melanoma and vitelliform dystrophy
Treatment
Currently, there is no approved treatment for torpedo maculopathy. Considering the rare possibility of developing choroidal neovascularization, it is recommended periodically monitoring these patients.
References
Golchet PR, Jampol LM, Mathura JR Jr, Daily MJ. Torpedo maculopathy. Br J Ophthalmol. 2010;94:302-6. https://pubmed.ncbi.nlm.nih.gov/19822914/
Parodi MB, Romano F, Montagna M, et al. Neovascularization in torpedo maculopathy assessed on optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retina. 2018;49:210-213. https://pubmed.ncbi.nlm.nih.gov/30457658/
Wong EN, Fraser-Bell S, Hunyor AP, Chen FK. Novel optical coherence tomography classification of torpedo maculopathy. Clin Exp Ophthalmol. 2015;43:342-8. https://pubmed.ncbi.nlm.nih.gov/25266677/
Tripathy K, Sarma B, Mazumdar S. Commentary: Inner retinal excavation in torpedo maculopathy and proposed type 3 lesions in optical coherence tomography. Indian J Ophthalmol. 2018;66:1213-1214. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6080473/