Medical History:
A 68-year-old female patient presented with complaint of blurry vision in her left eye for 2 months. In her history; 8 years ago she had bilateral cataract surgery.
Diabetes mellitus (+)
Systemic hypertension (+)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
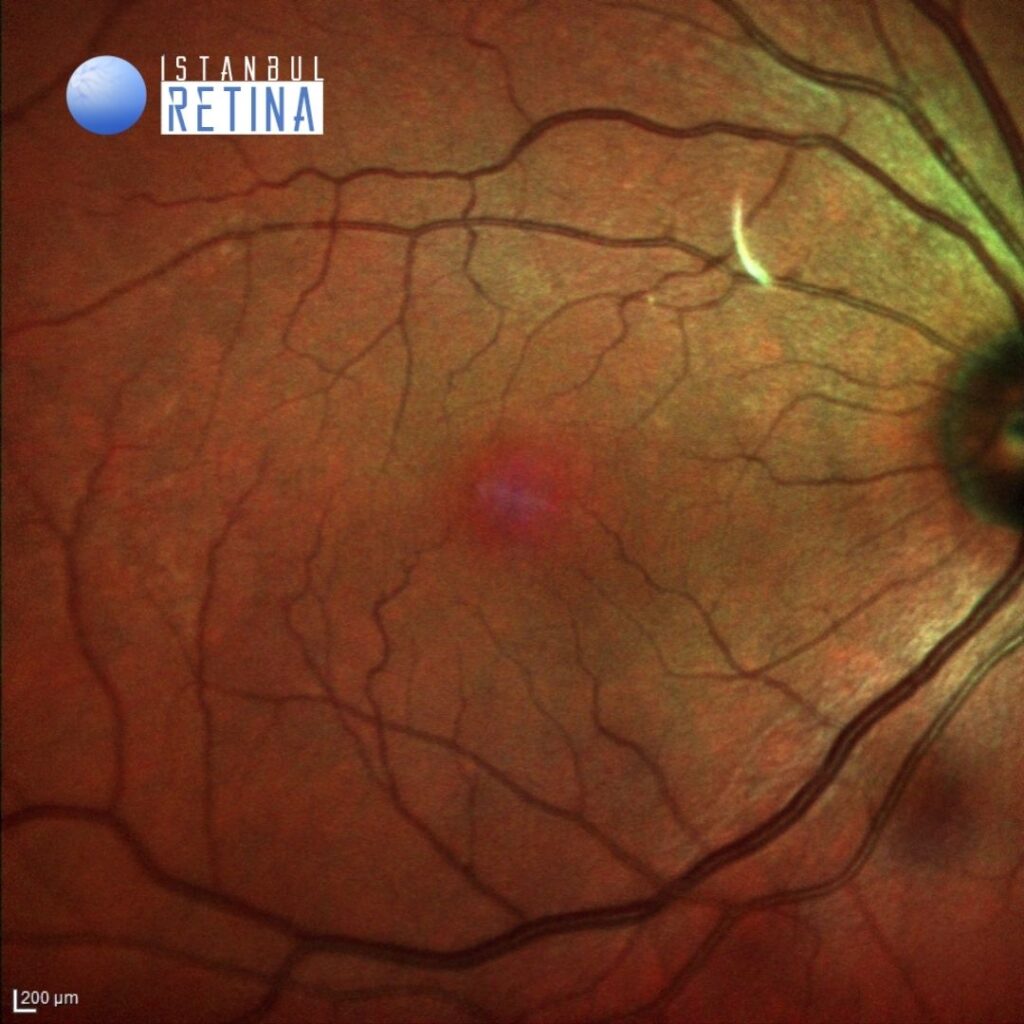
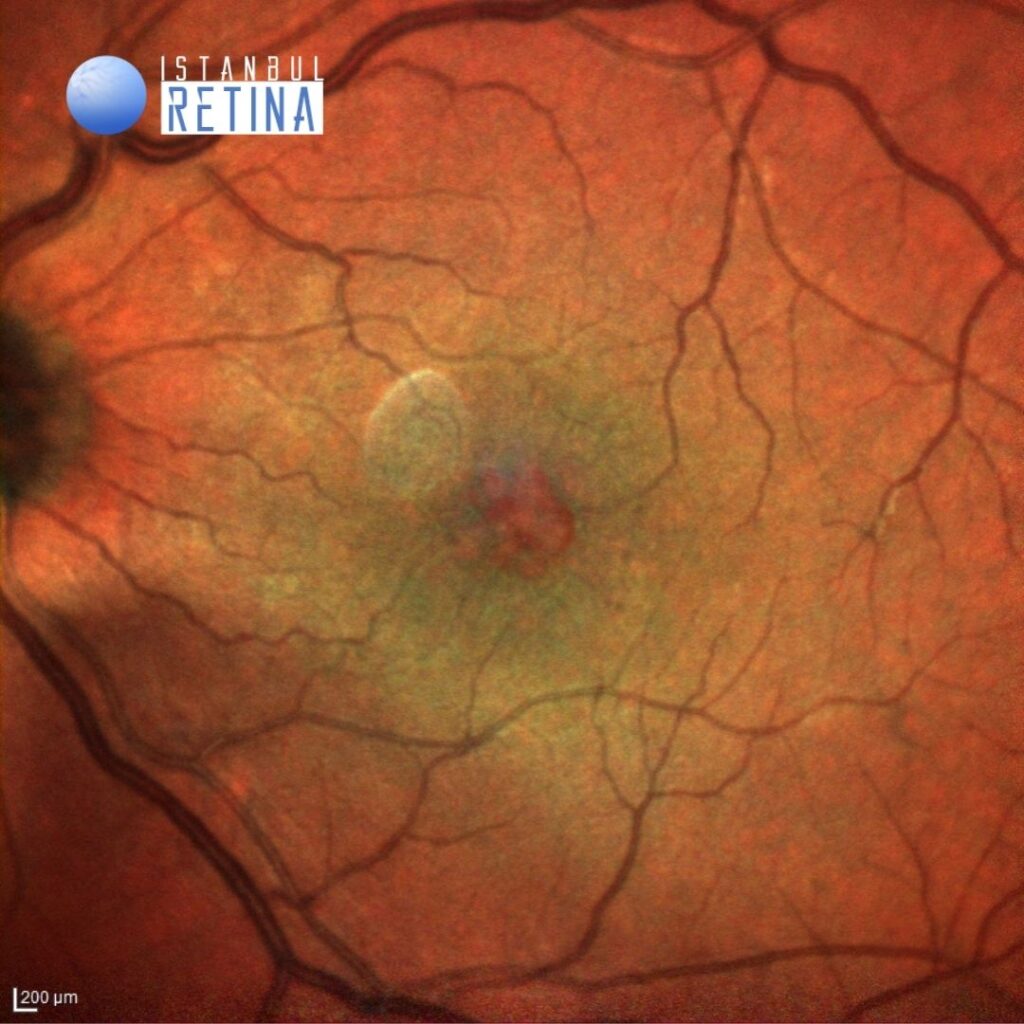
Best corrected visual acuity was 10/10 in the right eye and 3/10 in the left eye. Intraocular pressure was 17 mmHg in both eyes. Anterior segment examination revealed bilateral posterior chamber IOL (PCIOL) inserted into the capsular bag. Funduscopic examination revealed retinal cysts observed in foveal region in the left eye (Figure 1). The fundus in the right eye was normal.
Fluorescein angiography demonstrated normal angiographic pattern in the right eye and petaloid pattern of hyperfluorescence at the fovea in the late phases, optic nerve staining and patchy hyperfluorescence in the posterior pole in the left eye (Figure 2).
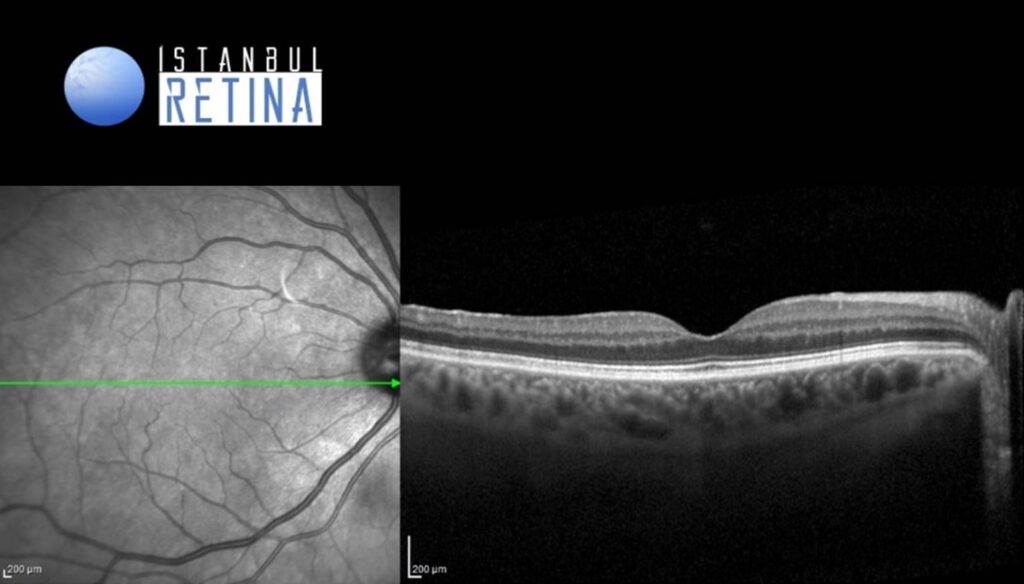
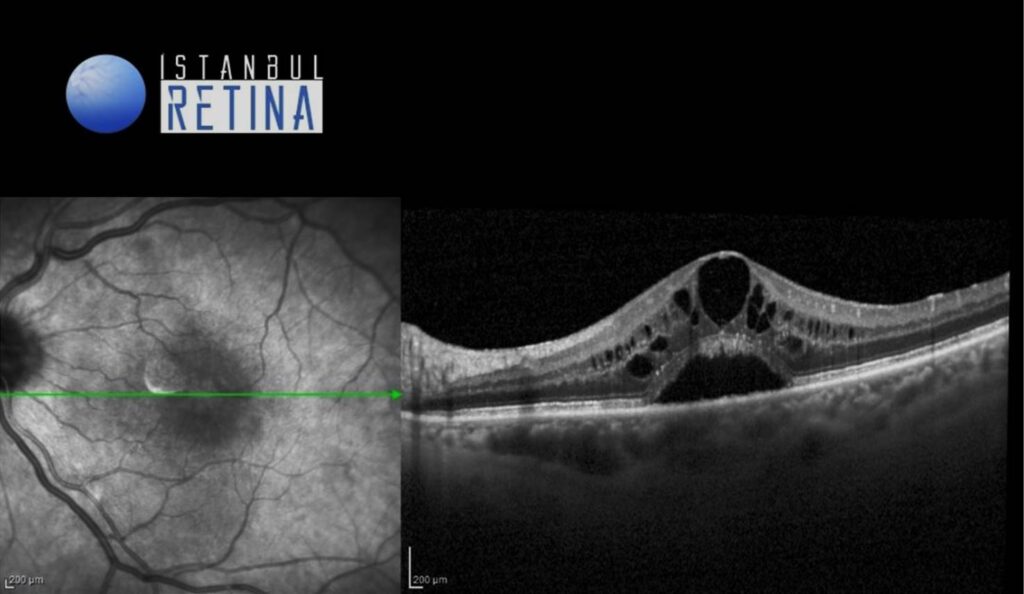
SD-OCT revealed normal foveal contour in the right eye and retinal thickening, intraretinal cystic spaces and subretinal fluid in the left eye (Figure 3).
Diagnosis
Very Late Onset Pseudophakic Cystoid Macular Edema
Pseudophakic cystoid macular edema (PCME), also known as Irvine-Gass syndrome, is one of the most common causes of visual loss after cataract surgery. Its incidence in patients with no risk factors has been reported to be 1%–2% . Although the pathogenesis of PCME is not completely understood, the contribution of postsurgical inflammation is generally accepted.
The onset is typically four to 12 weeks after surgery, reaching a peak incidence four to six weeks postoperatively. In a study of over 1,600 patients following cataract surgery, Henderson and colleagues found only three that were considered to be late onset (occurring more than three months after surgery). Mao and Holland define ‘very late onset cystoid macula oedema’ as that which occurs greater than five years following surgery.
Fluorescein angiography is the gold standard in diagnosing pseudophakic CME. Fluorescein angiography demonstrates petaloid leakage in the fovea, as well as patchy hyperfluorescence elsewhere in the posterior pole. The early hyperfluorescence in the central fovea is due to leakage of dye from the perifoveal capillary network. It typically increases in the mid-phase of the angiogram, leading to the characteristic petaloid pattern of hyperfluorescence at the fovea in the late phases. Usually there is late hyperfluorescence of the optic disc and helps to distinguish pseudophakic CME from other causes of CME such as diabetic macular edema and retinal vein occlusion.
Differential Diagnosis
Diabetic macular edema, retinal vein occlusion, hypertensive retinopathy, uveitis, topical prostaglandins analogs
Treatment
There is no standardized treatment for PCME. Although in most acute cases, PCME spontaneously resolve, the treatment of chronic pseudophakic CME remains a challenge. Corticosteroids and topical NSAIDs, either as monotherapy or combined therapy, are a commonly used first-line treatment approach. When this approach is ineffective, intravitreal application of corticosteroids and anti-vascular endothelial growth factor agents may be an option. In eyes with chronic PCME and vitreomacular traction, pars plana vitrectomy can be considered.
References:
1. Henderson BA, Kim JY, Ament CS, FerrufinoPonce ZK, Grabowska A, Cremers SL. Clinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatment. J Cataract Refract Surg 2007; 33: 1550–1558. https://pubmed.ncbi.nlm.nih.gov/17720069/
2. Mao LK, Holland PM. ‘Very late onset’ cystoid macular edema. Ophthalmic Surg 1988; 19: 633–635.https://pubmed.ncbi.nlm.nih.gov/3186172/
3. Jakob-Girbig J, Hahner L, Meller D. Very late onset Irvine-Gass Syndrom [Very late onset Irvine-Gass syndrome]. Ophthalmologe 2021;118:1267-1271. https://pubmed.ncbi.nlm.nih.gov/33237362/
4. Leon Nehmad. Late onset cystoid macular oedema presents a diagnostic challenge. Clin Exp Optom 2014;97:459–462. https://pubmed.ncbi.nlm.nih.gov/24985715/