Medical History:
A 40-year-old male patient presented with complaint of blurred vision in his right eye.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
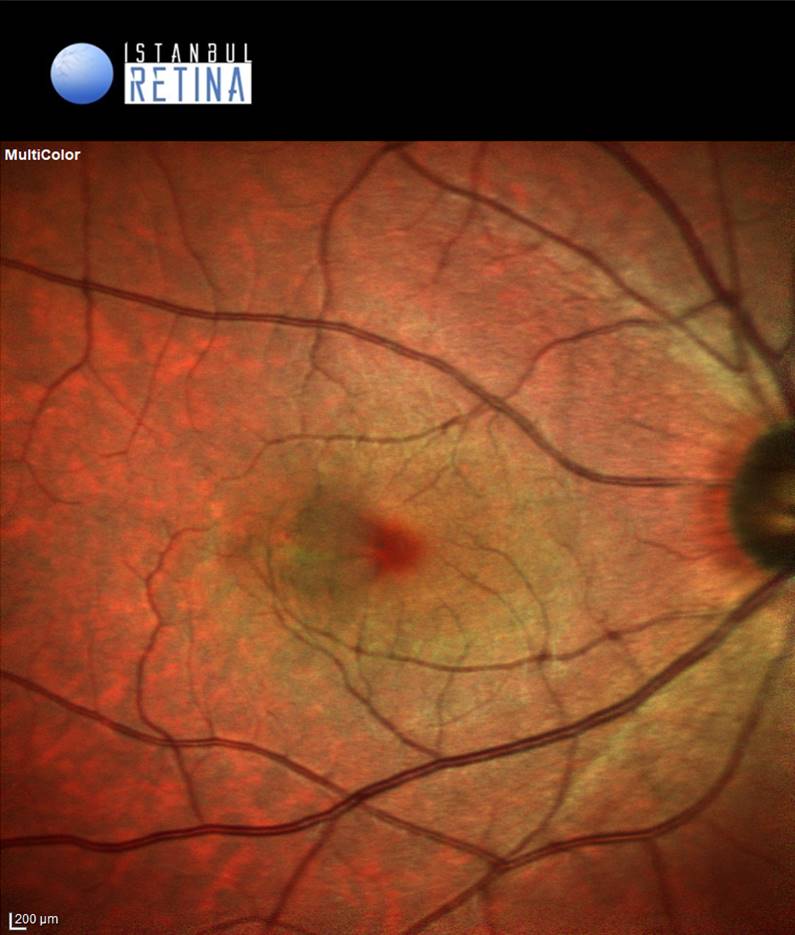
Best corrected visual acuity was 9/10 in the right eye and 10/10 in the left eye. Intraocular pressure was 17 mmHg in the right eye and 16 in the left eye. Anterior segment examination was unremarkable. Fundoscopic examination of the lef eye was normal. Fundoscopic examination of the right eye showed localized swelling temporal to the fovea (Figure 1).
.
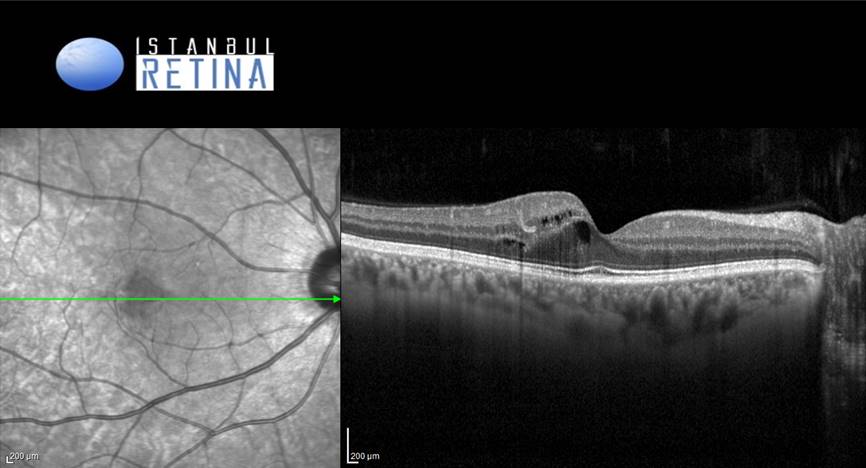
SD-OCT imaging of the right eye revealed hyperreflective lesion temporal to the fovea in the inner plexiform layer and intraretinal cystic spaces (Figure 2).
.
.
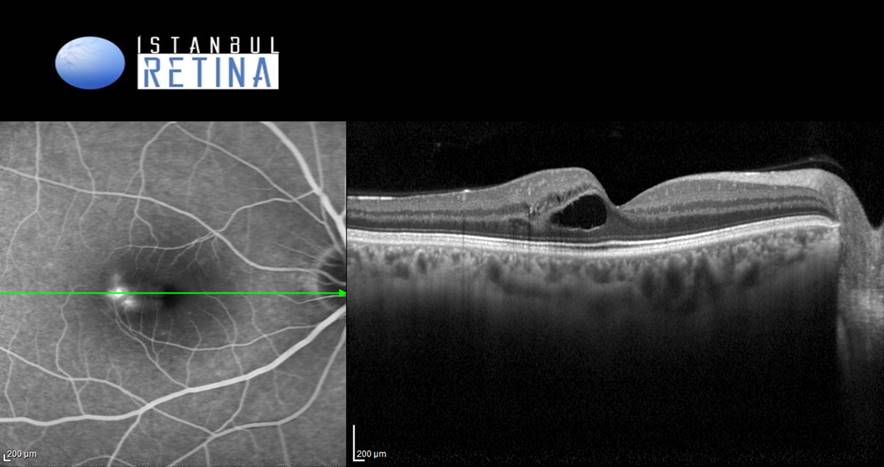
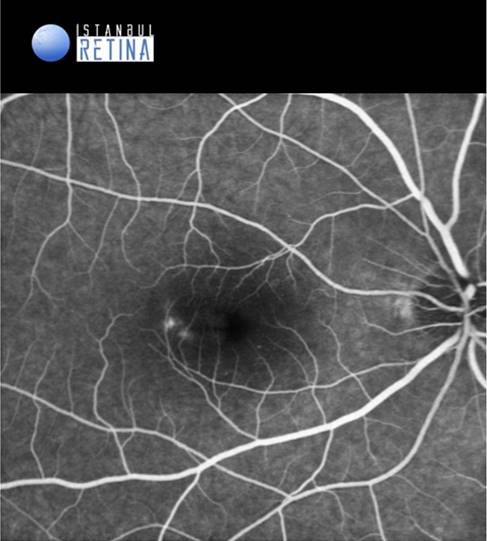
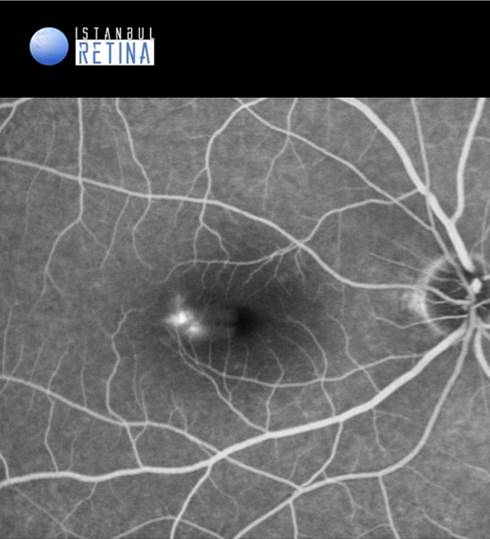
Fluorescein angiography showed hyperfluorescent lesion in the early phases (Figure 3A) and leakage in the late frames (Figure 3B) of the angiogram in the right eye.
Diagnosis
Perifoveal Exudative Vascular Anomalous Complex (PEVAC)
Perifoveal exudative vascular anomalous complex (PEVAC) appears as perifoveal isolated aneurysm, appearing similar to a large microaneurysm, associated with small retinal hemorrhages, intraretinal exudation, and in some cases hard exudates. Age at diagnosis is variable (46-90 years).
The etiology is unknown. PEVAC is not associated with diabetes mellitus, systemic hypertension and blood dyscrasias. There are no signs of exudative age related macular degeneration (AMD), diabetic maculopathy or sequellae from retinal vascular occlusive or inflammatory diseases.
On OCT, PEVAC appears as a round unilateral hyperreflective lesion with intraretinal cystic spaces without any indication of neovascularization. In most cases located between the outer plexiform layer and the inner nuclear layer, but may also be found in the inner plexiform later.
Fluorescein angiography demonstrates well-defined hyperfluorescent lesion with isolated aneurysmal dilation with variable leakage in the late frames. Indocyanine green angiography had the same lesion noted in fluorescein angiography without any leakage noted. Fluorescein angiography and indocyanine green angiography demonstrates no retinal or choroidal abnormalities in patients with PEVAC.
Differential Diagnosis
Type 1 macular telangiectasia (MacTel), neovasular AMD (type 3 neovascularization) macroaneurysm associated with other disorders such as retinal vein occlusion, diabetic retinopathy and or other systemic/inflammatory diseases.
Treatment
PEVAC demostrates wide clinical spectrum. Patients may be asymptomatic at baseline. Observation is recommended with Amsler grid monitoring. PEVAC lesions may regress spontaneously and even disappear over time. Visual decline occurring associated with cystoid macular edema (CME). No randomized control trials on the treatment of PEVAC. However, intravitreal anti-vascular endothelial growth factor injections can be used.
References:
1. Querques G, Kuhn D, Massamba N, et al. Perifoveal exudative vascular anomalous complex. J Fr Ophtalmol. 2011;34:559.e1-4. https://pubmed.ncbi.nlm.nih.gov/21550688/
2. Mrejen S, Le HM, Nghiem-Buffet S, et al. Insights into perıfoveal exudatıve vascular anomalous complex. Retina. 2020;40:80-86. https://pubmed.ncbi.nlm.nih.gov/30601390/
3. Smid LM, Verhoekx JSN, Martinez Ciriano JP, et al. Multimodal imaging comparison of perifoveal exudative vascular anomalous complex and resembling lesions. Acta Ophthalmol. 2021;99:553-558. https://pubmed.ncbi.nlm.nih.gov/33210824/