Medical History
A 55-year-old female presented with decreased visual acuity in the left eye.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
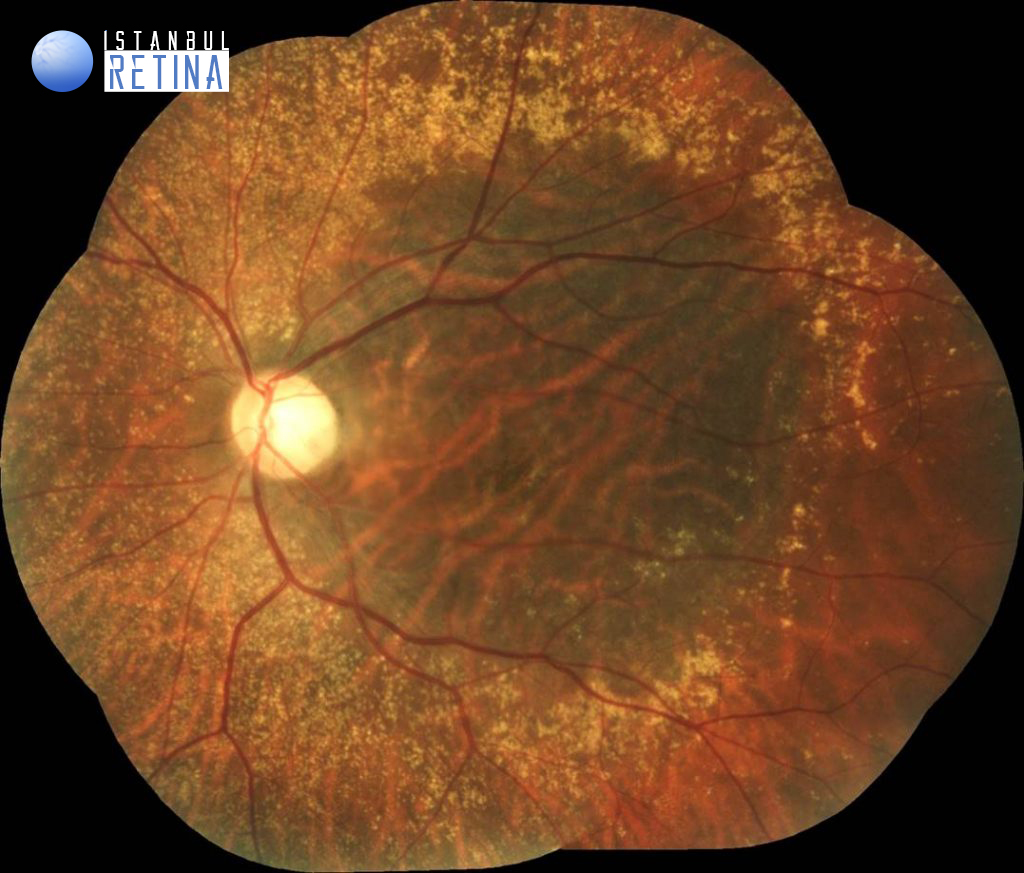
The best corrected visual acuity was 10/10 in the right eye and 1/10 in the lefte eye. Intraocular pressure was 16 mmHg in both eyes. The anterior segment examination was unremarkable. Fundus examination revealed bilateral, numerous, yellowish-white drusen-like deposits along the vascular arcades and nasal to the optic disc. In addition, a large serous macular detachment and optic pit located on the temporal side of the optic disc were observed (Figure 1).
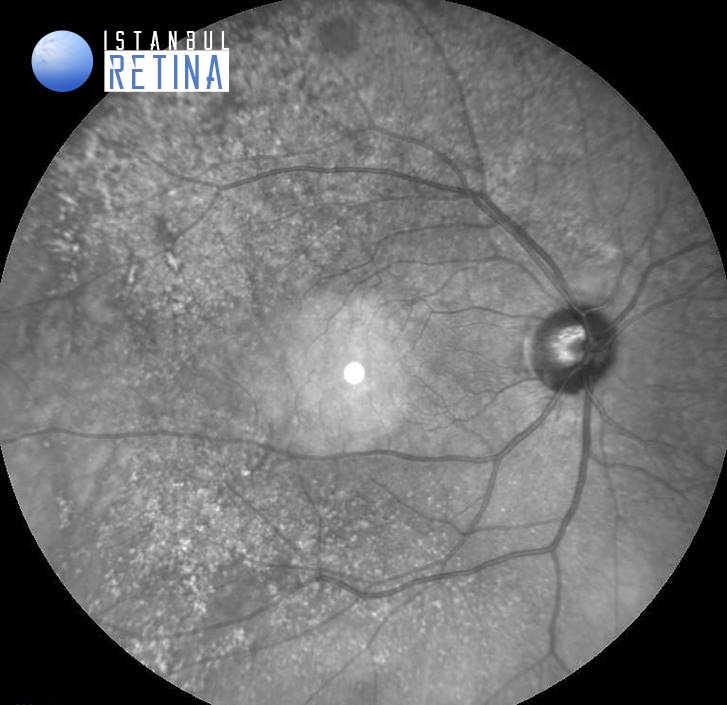
On infrared reflectance imaging drusen appeared primarily hyper-reflective. Due to RPE atrophy large choroidal vessels are clearly visible in the left eye (Figure 2).
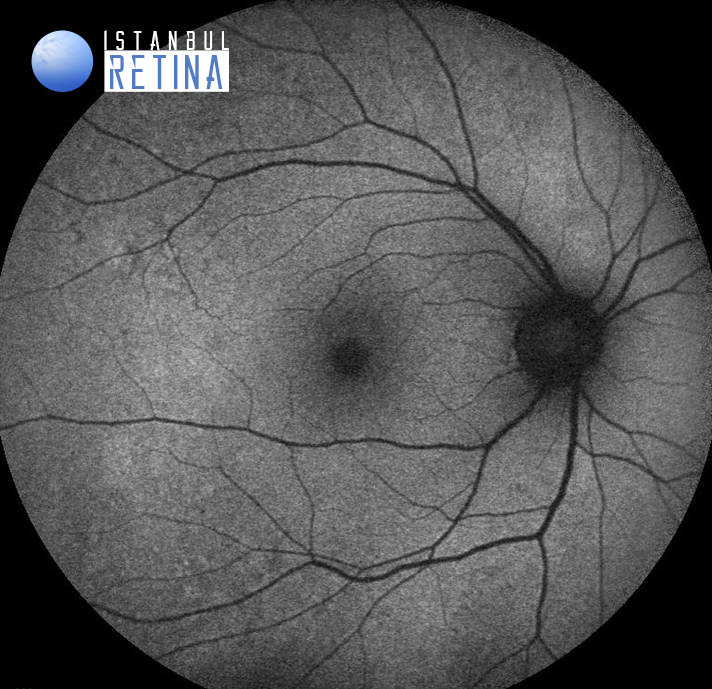
Fundus autofluorescence imaging revealed granular hypo- and hyper-autofluorescence at the posterior pole in the left eye (Figure 3)
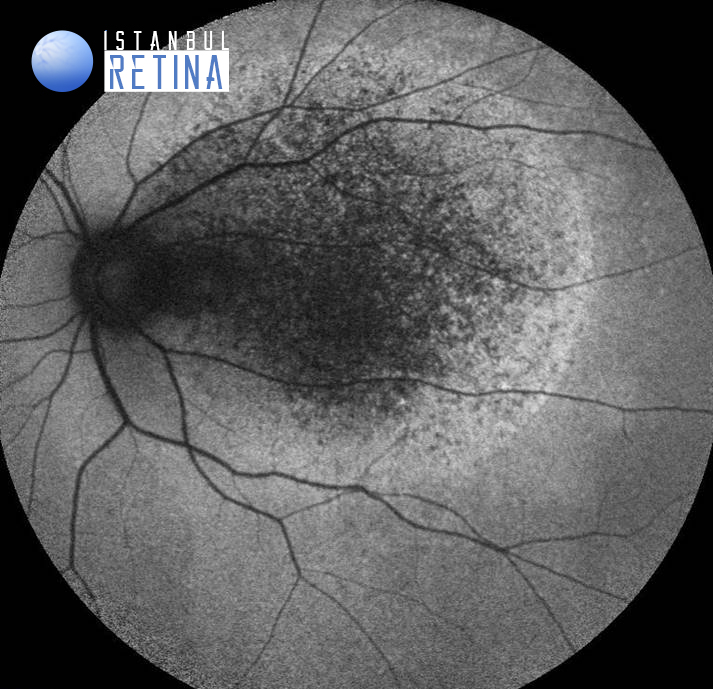
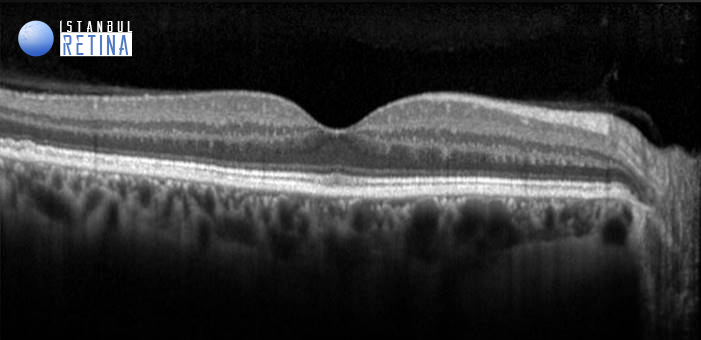
SD-OCT showed normal foveal contour in the right eye, and retinoschisis and serous macular detachment in the lefte eye (Figure 4).
Diagnosis
Sorsby’s Fundus Dystrophy and Optic Pit Maculopathy
Sorsby’s fundus dystrophy is a dominantly inherited disorder originally described by Sorsby in 1949. In some patients a confluent yellow deposit at the level of the retinal pigment epithelium is associated with the subsequent development of geographic atrophy or choroidal neovascularisation. In others, the most obvious change is drusen-like deposits seen along the arcades and nasal to the optic disc rather than at the central macula. Drusen centred over the fovea is not a frequent finding in this disorder, making the distinction between Sorsby’s fundus dystrophy and other forms of age related and genetically determined drusen (Malattia levantinese, Doyne’s honeycomb degeneration) relatively straightforward.
Congenital optic pits are thought to result from an imperfect closure of the embryonic fissure. The prevalence of optic pits is approximately 1:11,000. Maculopathy occurs in 25–75% of patients with an optic pit. The exact pathogenesis of the optic disc pit maculopathy is unknown. It has been hypothesized that submacular fluid originates either from the vitreous or the cerebrospinal fluid. Three patterns of maculopathy were noted on OCT: a combination of retinoschisis and serous macular detachment (80%), serous macular detachment only (12%) and retinoschisis only (8%).
Differential Diagnosis
Sorsby’s fundus dystrophy: Fundus flavimaculatus, fundus albipunctatus, age related macular degeneration, Malattia leventinese, Doyne’s honeycomb degeneration
Optic pit maculopathy: Central serous chorioretinopathy, subretinal neovascular membrane
Treatment
Currently, there is no genetic or targeted therapies to correct the underlying genetic mutation in Sorsby’s fundus dystrophy. Patients with Sorsby’s fundus dystrophy are managed conservatively with observation, unless a choroidal neovascularisation develops. Optic disc pit maculopathy resolves spontaneously in 25% of cases. Although observation for 3 months is generally recommended after the first examination, vitreoretinal surgery should be performed in case of increase in submacular fluid and a decrease in vision.
References
1. Sorsby A, Mason ME, Gardener A. A fundus dystrophy with unusual features. Br J Ophthalmol. 1949;33:67-97. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC510908/
2. Piguet B, Haimovici R, Bird AC. Dominantly inherited drusen represent more than one disorder: a historical review. Eye (Lond). 1995;9 ( Pt 1):34-41. doi: 10.1038/eye.1995.5. https://pubmed.ncbi.nlm.nih.gov/7713248/
3. Uzel MM, Karacorlu M. Optic disk pits and optic disk pit maculopathy: A review. Surv Ophthalmol. 2019;64(5):595-607. https://pubmed.ncbi.nlm.nih.gov/30797884/
4. Karacorlu M, Sayman Muslubas I, Hocaoglu M, Ozdemir H, Arf S, Uysal O. LONG-TERM OUTCOMES OF RADIAL OPTIC NEUROTOMY FOR MANAGEMENT OF OPTIC DISK PIT MACULOPATHY. Retina. 2016;36(12):2419-2427. https://pubmed.ncbi.nlm.nih.gov/27579729/
5. Karacorlu SA, Karacorlu M, Ozdemir H, Burumcek E, Esgin H. Optical coherence tomography in optic pit maculopathy. Int Ophthalmol. 2007;27(5):293-7. https://pubmed.ncbi.nlm.nih.gov/17487546/
6. Sanghi G, Padhi TR, Warkad VU, et al. Optical coherence tomography findings and retinal changes after vitrectomy for optic disc pit maculopathy. Indian J Ophthalmol. 2014;62(3):287-290. https://pubmed.ncbi.nlm.nih.gov/23619493/