Medical History
A 60-year-old male patient with progressive vision loss in both eyes was examined in our clinic.
Diabetes mellitus (-)
Systemic hypertension (+)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
Best corrected visual acuity was 8/10 in the right eye 3/10 in the left eye. Intraocular pressure was 10 mmHg in both eyes. Anterior segment and fundus examination were unremarkable in both eyes. Ishihara color vision test was normal in both eyes.
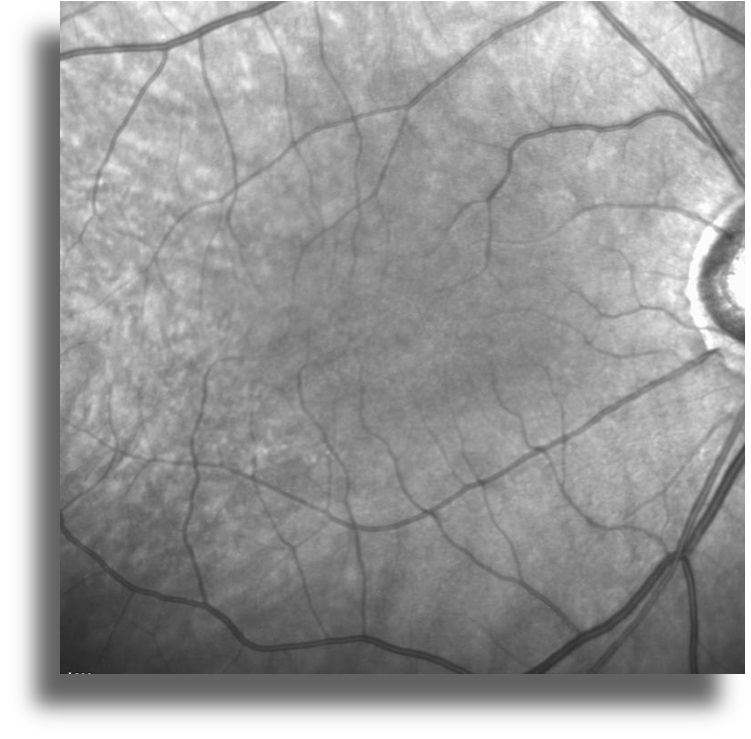
Color fundus imaging shows no abnormality in both eyes (Figure 1).


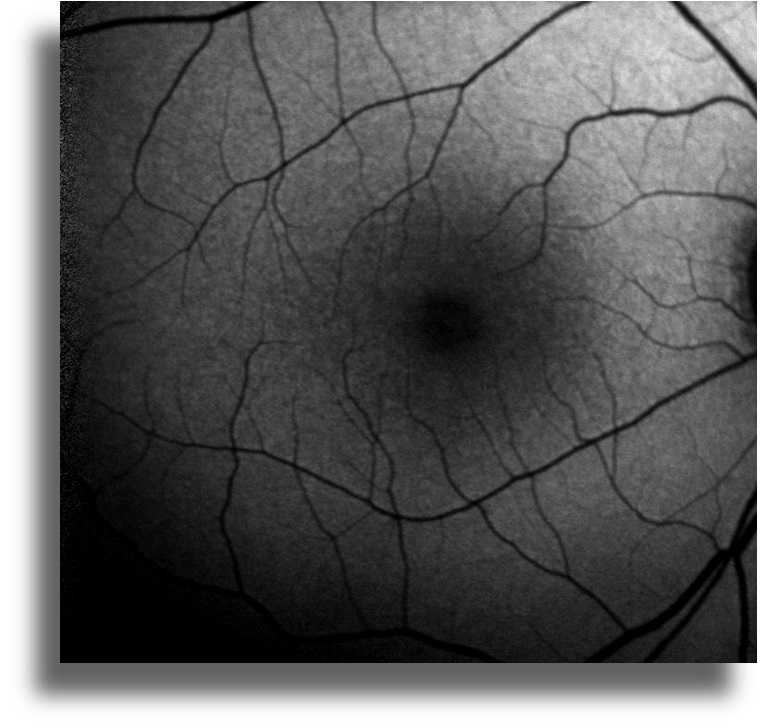
Infrared reflectance imaging shows no abnormality in both eyes (Figure 2)

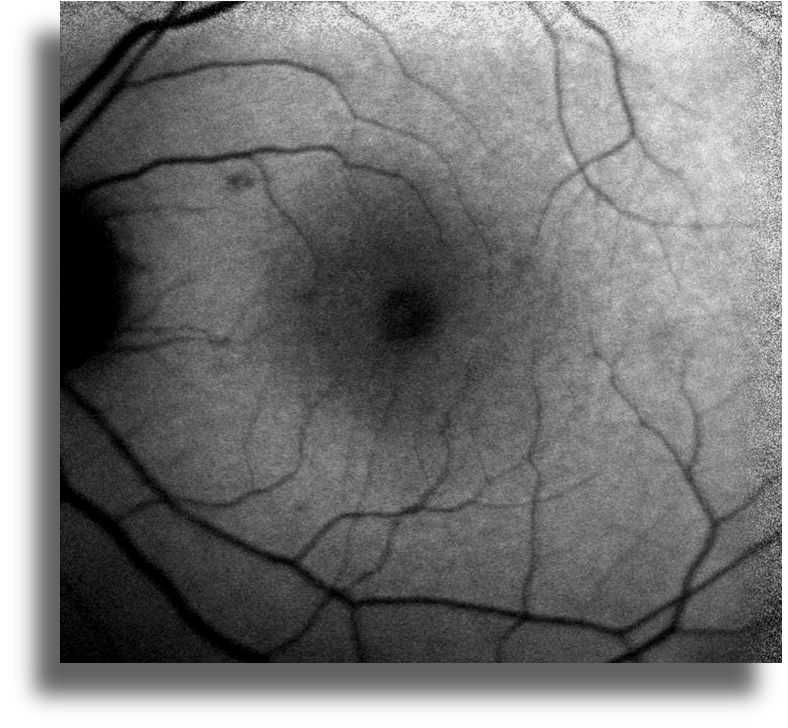
Fundus autofluorescence imaging shows no abnormality in both eyes (Figure 3)
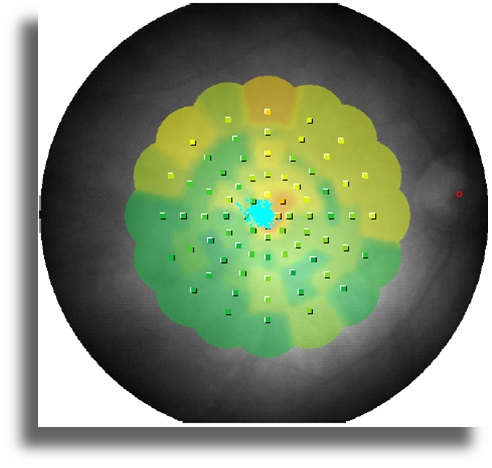
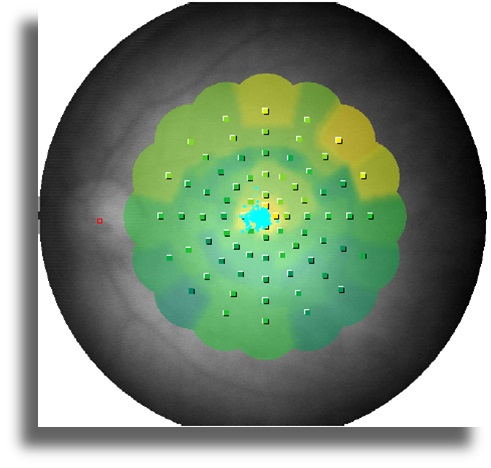
In the MP-1 Microperimetry test, retinal sensitivity was decreased in both eyes. Fixation was central and stable. Absolute scotoma area was not observed (Figure 4).
Electrophysiological testing
Pattern and flash VEP: Normal
ERG: A slight decrease in scotopic b wave amplitude, photopic responses are normal
EOG: Normal
mfERG: Disruption of waveforms in both eyes.
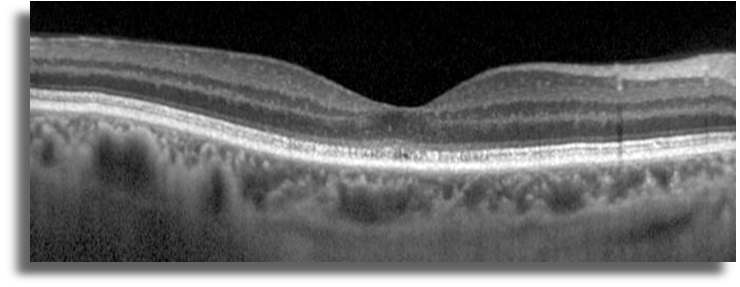
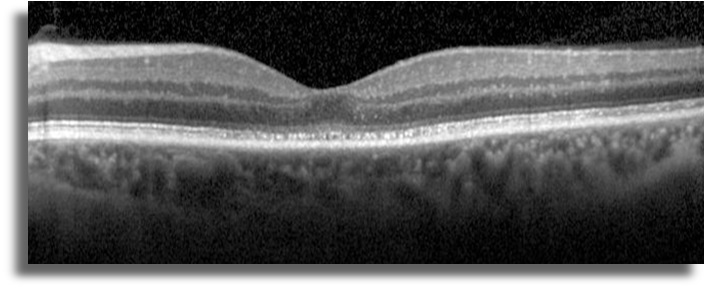
SD-OCT imaging shows disruption of photoreceptor layer in both eyes (Figure 5)
Anti Retinal Autoantibodies (+)
(WB Anti Retinal Autoantibody, WB Anti Optic Nerve Autoantibody, IHC Anti Retinal Autoantibody)
Differential Diagnosis
Cancer associated autoimmune retinopathy
The patient was directed to the oncology. No malignant tumors were detected in the systemic evaluation.
Diagnosis
Non-Neoplastic Autoimmune Retinopathy
References
- Uludag G, Onal S, Arf S, Sayman Muslubas I, Selcukbiricik F, Koc Akbay A, Molinas Mandel N. Electroretinographic improvement after rituximab therapy in a patient with autoimmune retinopathy. Am J Ophthalmol Case Rep. 2016 30;2:4-7.
doi: 10.1016/j.ajoc.2016.03.007


