Medical History:
A 52-year-female patient presented to our clinic complaining of decreased vision in both eyes since the last 20 days.
Diabetes mellitus (-)
Systemic hypertension (-)
Family history (-)
Smoking (-)
Trauma (-)
Examination Findings
Her best corrected visual acuity was 2/10 in both eyes. Intraocular pressure was 14 mmHg in the right eye and 13 in the left eye. Anterior segment examination was unremarkable. Dilated funduscopic examination revealed a pale, yellow-white, oval-shaped placoid lesion in the macular region of the both eyes macula (Figure 1). The optic disks and retinal vessels had a normal appearance. No inflammatory cells were observed in the vitreous cavity.

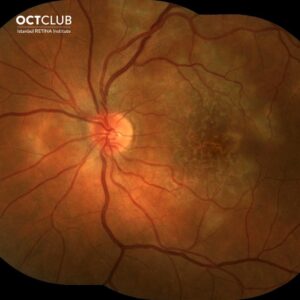
Fig. 1
Fundus autofluorescence revealed linear hypoautofluorescence surrounding the edges of hyperautofluorescent lesions in both eyes (Figure 2).
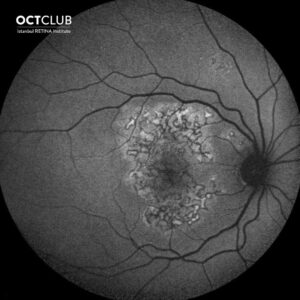
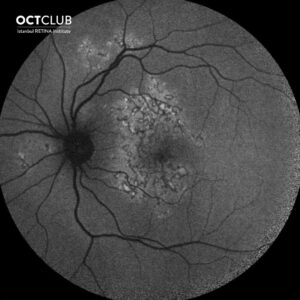
Fig. 2
Fluorescein angiography showed early hypofluorescence with late leakage at the margins of atrophic macular lesions in both eyes (Figure 3).
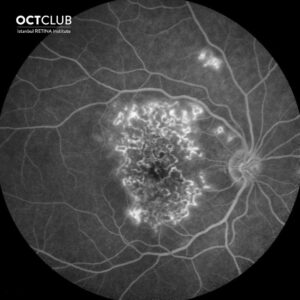

Fig. 3
Indocyanine green angiography was characterized by hypofluorescent maular areas from early to late frames in both eyes (Figure 4).
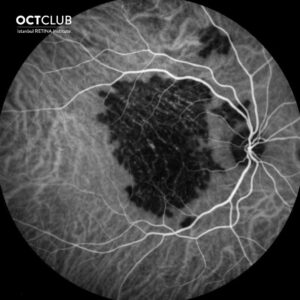
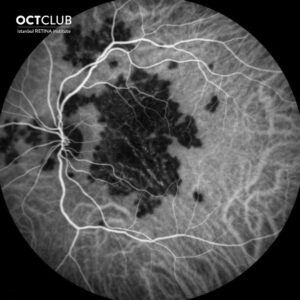
Fig.4
Optical coherence tomography (OCT) demonstrated hyper reflectivity in the outer retina with loss of inner segment and outer segment junction and loss of retinal pigment epithelium (RPE) in both eyes (Fig 5).
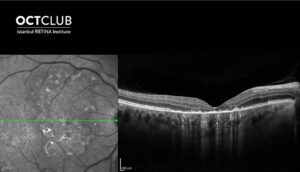
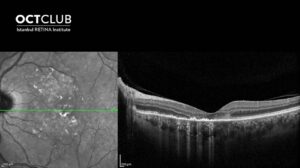
Fig. 5
Diagnosis
Macular Serpiginous Choroidopathy
Serpiginous choroiditis is a recurrent, asymmetrically bilateral inflammation of the choroid. This results in choriocapillaris and retinal pigment epithelium (RPE) loss, photoreceptor degeneration and subsequent vision loss. Initially described in patients with tuberculosis and syphilis, the disease was subsequently considered as idiopathic choroiditis. The term serpiginous‑like choroiditis and multifocal serpiginoid choroiditis have been used to differentiate serpiginous choroiditis due to tubercular etiology from classic serpiginous choroiditis.
Based on lesion morphology and characteristics, serpiginous choroiditis can be further subdivided into the following categories:
Peripapillary serpiginous choroiditis is the most common type of serpiginous choroiditi. The lesion in peripapillary serpiginous choroiditis is usually unifocal and occurs around the optic disc and progresses in a serpentine pattern centrifugally to involve macula.
Macular serpiginous choroiditis, though relatively uncommon, is a dreaded cause of vision loss due to early macular involvement and a higher risk of developing choroidal neovascularization.
Relentless placoid chorioretinitis is another term used to describe an unusual clinical entity resembling APMPPE and serpiginous choroiditis both clinically and angiographically with an atypical clinical course. In contrast to the lesions seen in APMPPE, which are usually limited to the posterior pole, lesions in relentless placoid chorioretinitis are usually numerous (ranging from 50 to 100) and involve the posterior pole, mid-periphery, and far-periphery, often predating or occurring simultaneously with macular involvement.
Differential Diagnosis
Multifocal chorioretinitis, APMPPE, toxoplasmosis and tuberculosis.
Treatment
Systemic or periocular corticosteroids are often used, but long-term anti-inflammatory treatment with a steroid-sparing agent (e.g., antimetabolites like methotrexate, mycophenolate mofetil, or azathioprine; cyclosporine A; or anti-TNF agents like adalimumab or infliximab) is typically required for recurrence prevention, after ruling out tuberculosis.
References:
Dutta Majumder P, Biswas J, Gupta A. Enigma of serpiginous choroiditis. Indian J Ophthalmol. 2019;67(3):325-333. https://pubmed.ncbi.nlm.nih.gov/30777946/


